Review Article - (2024) Volume 6, Issue 1
Background: The Human Immunodeficiency Virus (HIV) can be transmitted from HIV positive mothers to their child during pregnancy, at time of giving birth and breastfeeding. Majority of children infection with HIV is due to Mother To Child Transmission (MTCT). The prevalence of Mother To Child Transmission (MTCT) of HIV in pregnant HIV positive women with no intervention ranges from 15%-45%.
Objective: To assess the knowledge, attitude, Practice of Mother To Child Transmission of HIV (PMTCT) among pregnant mothers attending antenatal clinic at Pagak health center, South Sudan
Methodology: An institution based cross-sectional study was conducted from January 2023 to February 2023, investigated knowledge, attitude and practice towards PMTCT of pregnant mothers attending antenatal clinic at Pagak health center, upper Nile state, Maban county. Data were entered to Epi-info and were analysed using SPSS version 26. Association between dependent and independent variables were examined by using bivariate and multivariable logistic regression models and were reported as unadjusted Odds Ratio (OR) and Adjusted Odds Ratios (AOR) with 95% Confidence Interval (CI). In addition Pvalue (<0.05) were used to examine statistical significance.
Result: Pregnant women whose educational status is secondary and above had four times knowledge about MTCT than their counter party (AOR=4.50: 95% CI (1.18-17.07)). Pertaining ANC visit, pregnant women who had repeated visit, had three fold knowledge about MTCT than their counterpart (AOR=3.58: 95% CI (1.49-8.60))
Conclusion: This study concluded that educational status and numbers of ANC contacts are crucial for the knowledge, attitude and practise on PMTCT. Moreover, the study explored that the pregnant women had moderate knowledge, attitude, and practise as we compared to the similar study conducted in the neighbours countries. Intervention and improvement are much needed to extend the PMTCT services to larger scale. Girls’ education is more important as to understand PMTCT and result in to good health of both mother and baby.
PMTCT • ANC • KAP • Education • Good health
ANC: Antenatal Care; AOR: Adjusted Odds Ratio; CI: Confidence Interval; EBF: Exclusive Breastfeeding; HIV: The Human Immunodeficiency Virus (HIV); KAP: Knowledge, Attitude and Practice; MTCT: Mother To Child Transmission of HIV; PMTCT: Prevention of Mother To Child Transmission of HIV; PITC: Provider Initiated Testing and Counseling; PITC UNICEF: United Nations Children’s Fund; WHO: World Health Organization
Background
The Human Immunodeficiency Virus (HIV) can be transmitted from HIV positive mothers to their child during pregnancy, at time of giving birth and breastfeeding. Majority of children infection with HIV is due to Mother To Child Transmission (MTCT) [1,2]. The prevalence of Mother To Child Transmission (MTCT) of HIV in pregnant HIV positive women with no intervention ranges from 15%-45%. Intervention such as Antiretroviral Therapy (ART), postexposure prophylaxes and Prevention of Mother To Child Transmission (PMTCT) service can reduce the proportion of MTCT to less than 5%.
Since the emergence HIV pandemic, it is estimated that 84.2 million (64.0 million-113.0 million) people have been infected with the HIV virus and about 40.1 million ± 7.5 million people have died of HIV. Globally, 38 million ± 4.5 million people were living with HIV at the end of 2021. An estimated 0.7% ± 0.1% of adults aged 15 years-49 years worldwide are living with HIV, even though the encumbrance of the epidemic continues to vary considerably between countries and regions. Among the WHO regions, the African region is the most severely affected, with nearly 1 in every 25 adults living with HIV and accounting for more than two-thirds of the people living with HIV worldwide [3,4].
However the risk of vertical transmission is significantly reduced with effective HIV treatment and a well handled delivery, United Kingdom is the best example where vertical transmission from pregnant women with diagnosed HIV has fallen to 0.3% [5].
Statement of the problem
HIV continues to be a major global public health issue. After four decades of its emergence, in the year 2021 children of fewer than 15 years of age of living with HIV, acquiring HIV and dying from HIV related causes were 1.7 million, 160,000 and 98,000 respectively. In the same year women who live with HIV, acquiring (newly infected) HIV and dying from HIV related causes were 19.7 million, 64,000 and 240,000 respectively. Mother To Child Transmission (MTCT) of the virus can occur in the uterus during pregnancy, in the birth canal during delivery (intrapatum), and after birth through breastfeeding [6,7]. In low income society prevention of mother to child transmission is complicated since breast feeding is the only available means of feeding the new born. The enormous benefits of breastfeeding such as preventing malnutrition, saving money, energy, cost and decreasing the incidence of disease such as diarrheal disease and respiratory infection will be missed. In the absence of any intervention, the risk of Mother To Child Transmission (MTCT) of HIV among non-breast feeding populations is 15%-30%; breastfeeding by an infected mother increases the risk by 5%-20% to a total of 20%-45%. Some studies showed that breast feeding duration also increase the risk of transmission by 30%-45% if there is breast feeding through 18 months-24 months.
In some studies, the researcher argued that the knowledge of HIV transmission confined to sexual transmission of HIV, while knowledge on prevention of vertical transmission is inadequate among women of reproductive age [8,9]. Therefore, the purpose of this study is to assess the knowledge, attitude and practice on prevention of mother to child transmission of HIV among pregnant women in Pagak. By doing so the study will uncover the knowledge attitude and practice gap and help to design effective strategies to prevent mother to child transmission of HIV and to promote appropriate infant feeding practice.
Prevention of mother to child transmission of HIV is the most effective intervention that averted pediatrics infection from 800,000 new pediatric infections to less than 160,000 new HIV infections in children per year [10]. The most crucial strategy to prevent MTCT of HIV infection is through creating public awareness towards HIV by educating its routes of transmission, methods of prevention and its consequences if acquired. Avoiding HIV infection among women of reproductive age bears great proportion of reducing the transmission of HIV to infants [11].
Thus, this study will contribute to fill the information gap, and in the design of strategies to prevent mother to child transmission of HIV and to promote appropriate infant feeding practice in the study setting and the country at large.
Significance of the study
Vertical transmission is the single most important cause of HIV infection among children. This study focuses in assessing the knowledge, attitude and practice of the pregnant women towards PMTCT. Women knowledge attitude and practice is towards PMTCT is a corner stone for reducing transmission of HIV from mother to child. Therefore, this study identifies the gaps in knowledge, attitude and practice of the pregnant women towards PMTCT in the study area.
More over the finding of this study will be helpful to professionals working on PMTCT to improve their roles in providing quality care. It will be a good input for policy makers to improve their policy towards increasing access to integrated and comprehensive prevention mother to child transmission program. Since there is no previous study in this study area, the finding of this study will be a base line for other researchers.
Infant feeding option for a baby born from HIV positive women
The ultimate objectives of infant feeding counseling sessions, should emphasis on helping HIV positive mothers to reduce HIV transmission through breastfeeding in clinical/subclinical mastitis, oral thrush and avoiding mixed feeding during the first 6 months of life is crucial for preventing MTCT of HIV. Effective counseling sessions during breastfeeding could focus on adherence counseling about every safe alternative, ways of feeding their babies in to prevent both mothers to child transmission and malnutrition. It should incorporate the timely period of weaning assuming appropriate complementary foods are available to prevent malnutrition [12,13].
The feeding options recommended for infants of HIV positive women are: Exclusive breastfeeding, expressing and heating breast milk or exclusive breastfeeding by wet-nurse who is HIV negative, or exclusive replacement feeding (avoidance of all breast-feeding).
Exclusive Breastfeeding (EBF) is defined as giving breast milk only to the infant, without any additional food or drink, not even water in the first six months of life, with the exception of mineral supplements, vitamins, or medicines. When Exclusive Breastfeeding (EBF) is backed by ART it decreases HIV transmission rate to less than 1%. Hence, parallel administration of EBF with ART not only reduces vertical transmission of HIV but also reduces child mortality, especially in areas where resources are limited.
The risk of vertical transmission increases with inconsistent maternal ART adherence. In poor settings where provision of ART is unreliable and or where maternal adherence is poor, this may result in transmitting HIV to children who are still breastfeeding.
Counseling and testing
HIV testing during pregnancy provides an entry point to PMTCT, treatment, care and support services when women are diagnosed with HIV. However, low uptake of HIV testing has been a challenge for PMTCT and subsequent HIV treatment, care and support services. Poor knowledge about MTCT, low maternal education level, fear stigma, and poor access to health services are the factors that affect uptake of HIV counseling and testing. A study showed that an estimated 30% of livings with HIV were unaware of their HIV status at the end of 2016.
Provider Initiated Testing and Counseling (PITC) is a good entry point for preventing the transmission of HIV from mother to child, even though studies are limited in this area and PITC is not widely accepted in low and middle income countries. Studies conducted in other regions of Ethiopia revealed different rates of PITC acceptance with some contradictory factors [14].
A study conducted in Kakamega district, Kenya and Dodoma rural district of Tanzania shows that 89% and 75.2% of HIV positive pregnant women satisfy with PMTCT counseling services respectively. Again a study conducted in Dodoma rural district of Tanzania shows that 76% of clients were satisfied with privacy when accessing services.
Knowledge attitude and practice on MTCT
Different studies have been done in different part of the world about knowledge attitude and practice of the pregnant women towards mother to child transmission of HIV. However many literatures supports that there is a big knowledge and practice gap from region to region. Much has to be done to maintain mothers knowledge, attitude and of all to promote the use of ART and other PMTCT of HIV methods through organized intervention programs as well as by ensuring the supply of the ART medications used for PMTCT of HIV beside the treatment of established infection.
A study conducted in north India, in district Srinagar, showed that majority of the study subjects (91.5%) and their spouses (74.9%) were tested for HIV infection. Among the study participants, majority (98.4%) had shared the result of HIV test with their spouse. Pertaining to HIV testing 96.4% and 77.3% had favorable attitude towards HIV testing among pregnant women and their spouses respectively. Majority (90.2%) agreed with that proper utilization of PMTCT services will eventually decrease the transmission of HIV infection to the newborn. Regarding delivery attendant 94.3% study participants had a favorable attitude towards delivery of HIV positive women by a skilled person. Whereas; Only 38.5% of the study subjects agreed that HIV positive mother should get ARV therapy during pregnancy and a very few subjects (12.3%) agreed to avoid breastfeeding the child to reduce risk of transmission of HIV infection to the child [15].
A study conducted in Southern Ethiopia, on knowledge attitude and practice of mother to child transmission of HIV among pregnant women attending ANC revealed that three-fourth (75.3%) knew that HIV can be transmitted from infected mother to her child. However, when a women asked the time of HIV transmission from infected mother to her baby 100 (58.8%) said during pregnancy, 80 (47.1%) replied during labor and delivery, 115 (67.6%) replied during breastfeeding while 51 (30%) do not know the time of transmission. Pertaining to ways of preventing HIV transmission from infected mother to her child, 87 (51.2%) of the respondents respond that it is possible to prevent MTCT by giving HIV medication during pregnancy, 62 (36.5%) by giving HIV medication to the baby and 49 (28.8%) do not knew. In this study about 112 (65.9%) of the respondents has good knowledge about MTCT of HIV/AIDS.
Another study conducted at Juba teaching hospital showed that only one-third (30.7%) of the participants had sufficient knowledge on when to start prophylaxis of MTCT (PMTCT). Half of the pregnant women (51%) showed positive attitudes toward PMTCT measures. Pertaining to practice of counseling and testing 231 (92%) of pregnant women had received counseling for HIV, with 78.4% of them reported being tested for HI.
A research on awareness and knowledge on timing of mother to child transmission of HIV among women in Southern Ethiopia found that only 60.7% were aware of the risk of MTCT. The possibility of MTCT during pregnancy, delivery and breastfeeding was known by 48.4%, 58.6% and 40.7% of the respondents, respectively. The proportion of women who were fully knowledgeable on timing of MTCT was 11.5%. Women’s full knowledge on timing of MTCT was associated with maternal education and being government employee [16].
A study conducted from neighboring country, Sudan, found that only few women knew about the Mother To Child Transmission (MTCT) of HIV. Among those who knew, no one indicated that MTCT might occur during labor. In fact most women believed that HIV/AIDS is a serious and fatal condition for them and also for their children. Unlike other studies, they believed they were susceptible to HIV/AIDS as a result of cesarean section. Some women in this study believed that HIV testing was perceived as an additional burden of anxiety and worry. Confidentiality issues were mentioned by some women as crucial factors affecting willingness to commence HIV testing at a health facility during pregnancy.
Another study which has been conducted in North West part of Ethiopia revealed that all of the respondents had heard about HIV/AIDS. More than three fourths, 390 (76.5%) of the women had knew their sero status. Nearly one-third, 160 (31.4%), of the respondents were knowledgeable on MTCT of HIV. When respondents were further asked to identify the sources of information and health professionals were the most frequently mentioned source of information, 402 (78.8%) followed by from friends and relatives 229 (44.9%). Pertaining the period of vertical transmission of HIV, four hundred ten (80.4%) knew that HIV can be transmitted from an infected mother to her baby of whom, 326 (63.9%) responded that MTCT of HIV could be occurred through breast feeding and 23 (5.5%) didn’t know the exact period of HIV transmission.
A study conducted in Southwestern Nigeria, revealed that almost all the respondents, 419 (99.8%), had heard about HIV/AIDS. Three hundred and eighty seven (92.1%) believed a mother can infect her child with HIV, while 292 (69.5%), 333 (79.3%), 363 (86.4%), and 239 (56.9%) agreed that MTCT of HIV takes place in utero, during delivery, through breastfeeding, and through invasive tests, respectively. In this study those who discussed about the issues of HIV testing in current pregnancy with their husband were 132 (56.9%). Regarding the perception of their husband on HIV screening, 148 (63.8%) wanted to have couple testing, 34 (14.7%) wanted only the woman to be tested, 10 (4.3%) did not want to be tested either and the other 34 (14.7%) did not want to respond. Similar study that has been studied in Tanzania on awareness and knowledge about HIV and PMTCT in pregnant women, in southwestern Tanzania showed that 67% had knowledge on MTCT during pregnancy and 78% knew the association between breastfeeding and mother to child transmission.
Another study conducted in Hawassa on practices of PMTCT among women attending ANC clinic prevention of mother to child transmission and factors affecting its practice among women were assessed using different explanatory variables. Among the respondents, 223 (96.1%) have been tested for HIV. Among these, 52 (23.3%) tested three months ago, 13 (5.8%) tested six months ago, 41 (18.4%) tested one year ago and 117 (52.5%) [17].

Figure 1: Conceptual framework.
Objective
General objective: To assess the knowledge, attitude, Practice of Mother To Child Transmission of HIV (PMTCT) among pregnant mothers attending antenatal clinic at Pagak health center, South Sudan.
Specific objective
• To determine the knowledge of prevention of mother to
child transmission of HIV/AIDS among pregnant mothers
attending antenatal clinic at Pagak health center, South Sudan.
• To examine the attitude towards voluntary counselling and
testing and prevention of mother to child transmission of
HIV/AIDS among pregnant mothers attending antenatal clinic
at Pagak health center, South Sudan.
• To assess practice of prevention of mother to child
transmission of HIV/AIDS among pregnant mothers attending
antenatal clinic at Pagak health center, South Sudan.
Study area and setting
Pagak is a town in South Sudan in Upper Nile state, a few kilometers from Jikawo (Jikawo is a woreda in Gambela Region, Ethiopia) across the Ethiopian border. Maban County (which means the people of the land) is a county located in the Upper Nile state of South Sudan. Its coordinates in the map is 8°29′N 34°01′E until 2017 Pagak served as headquarters for SPLA-IO rebels. Pagak has an estimated population of 34 thousand and total area of 8 square kilometers [18].
Study design
An institution based cross sectional study was conducted from 1st January 2023 to 1st February 2023. Investigated knowledge, attitude and practice towards PMTCT of pregnant mothers attending Antenatal clinic at Pagak health center, upper Nile State, Maban County.
Population
Source population: The source population for this study was all pregnant women living in Pagak town at the time of data collection.
Study population: The study population for this study was those women who were selected by systematic sampling techniques using the list of pregnant women for registration book as a sample frame.
Eligibility criteria
Inclusion criteria: All pregnant women who attend ANC at Pagak health center at the time of data collection and who were voluntarily participants were included.
Exclusion criteria: Pregnant women who were health professionals, too sick in labor pain or delivery were excluded.
Sample size determination
The actual sample size for the study was determined by using single population proportion formula for single proportion population. Since there is no previous study in this area, 50% prevalence to get the maximum sample size at 5% marginal error with 95% confidence [19].
Then using these assumptions the sample size was calculated by applying the formula of single population proportion.
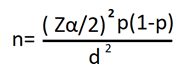
n=The required sample size.
P=Assumed proportion knowledge attitude and practice towards PMTCT.
Z=Standard score corresponding to 95% confidence interval.
d=Allowable marginal error.
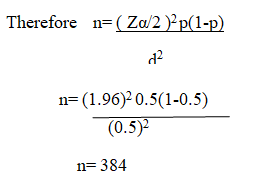
Since the population is less than 10,000 in the study period we use the correction formula to estimate final sample size (nf)
=384/(1+384/170)
=118
Data collection instrument
A structured questionnaire adapted from different literatures was first prepared in English in such a way that it includes all the variables to meet the objectives, The questionnaire was first prepared in English and then translated into Nuer language for better understanding by respondents. The Nuer version of the questionnaire was translated back to English language to check for its consistency. The data collection tools were pre tested on another health center which has similar set up with our study area before the initiation of the main study. Findings and experiences from the pre-test were utilized in modifying the interview [20].
The questionnaire consists of five parts with a total of 37 questions. The first part is about socio- demographic characteristics of the study participants, and composed of 6 questions. The second part is about past obstetric history and other part consists of questions raised for assessment of PMTCT, attitude, and practice and health service related. Questions about past obstetric history include gravidity, parity, number of children and decision: Questions about knowledge, attitude and practice were 9, 9 and 6 respectively.
Data collection procedure
Three nursing students were recruited as data collectors; one midwife was recruited as supervisor. All data collectors and supervisors were oriented for 2 days on data collection process based on the guide that was developed by principal investigator for data collectors and clarifying how to interview the questionnaire. They were allowed to fill the questionnaire and later discussion was made in all contents of the format and areas of difficulties were revised.
Additionally, they were trained on their responsibilities for describing the purpose of the study, giving orientation, telling clients the importance of honest and sincere reply, on responding to questions. The principal investigator and the coordinator strictly follow the overall activities for each activity on daily base to ensure the completeness of questionnaire, to give further clarification and support for data collectors.
Study variables
Dependent variable: Knowledge attitude and practice towards PMTCT.
Independent variable: Socioeconomic and demographic factors:
• Age
• Marital status
• Religion
• Educational status
• Monthly income
Obstetric factors:
• Parity
• History of still birth
• Number of children
• Live birth
Husband’s factors
• Husband’s occupation.
• Husband’s educational status.
Health service related factors:
• ANC follow up.
• Provision of counselling service or health education on HIV/MTCT/infant feeding.
Source of information about HIV/MTCT and infant feeding:
• Mass media
• Health workers
• Friends (relatives)
Data quality assurance
Questionnaire was prepared in English version and translated in to Nuer language and back to English to ensure consistency. Before the initiation of the main study pre-test was carried out on 5% of the calculated sample size in the Health center which are not selected in the study in order to check understandability, clarity and completeness of the questionnaire. Based on the finding of the pre-test the questionnaire was modified as necessary. Data collection was obtained by trained health science students from the nearby college. To control the quality of the data processing, the data was cheeked for its completeness before data entry and the cleaning process was done by running simple frequency after data entry for its consistency. The inconsistent data was checked referring the hard copy of the questionnaire.
Data processing, analysis and Interpretation
After the data collection, each questionnaire was checked for its completeness. Data entry, cleaning and coding was done by Epi Info version 3.5.4 statistical software package and exported to SPSS window version 26 for analysis. Associations between variables were assessed by using odds ratio, 95% confidence intervals. Multiple logistic regressions will also be used to adjust for possible confounding variables. Corresponding Pvalue of <0.05 was considered as statistically significant at 95% of confidence interval. Tables, bar graphs, pie charts and cross tabulations were used to present the data.
Bivariate logistic regression analysis was used to identify factors associated with knowledge, attitude and practice of PMTCT. Variables significant in the bivariate analysis were then entered into a multivariate logistic regression analysis [21-27].
Dissemination and utilization of results
Results of the study were disseminated to the ministry of health of South Sudan, upper Nile State, and Maban County. The findings were presented in different seminars, meetings and workshops and will be published in a scientific journal. Hard and soft copy will be available in the library of south Sudan Universities for graduate students as well as for other concerned [28,29].
Operational definitions
Knowledge: Knowledge of PMTCT means the basic information that the mothers have regarding PMTCT.
Good knowledge: Refers to those participants who respond correctly to knowledge questions and score above the median value.
Poor knowledge: Refers those participants who correctly respond to knowledge questions and score median value and below the median value.
Attitude: It is an opinion of study participants towards PMTCT.
Positive attitude: refers to those participants who respond correctly to attitude questions and score above the median value.
Negative attitude: Refers to those participants who respond correctly to attitude questions and score median value and below the median value.
Practice: A woman’s activities in relation to PMTCT.
Good practice: Refers to those participants who respond correctly to practice questions and score above the median value.
Poor practice: Refers those participants who correctly respond to practice questions and score median value and below the median value.
Socio-demographic characteristics
A total of 113 women responded to the questionnaire, with a response rate of 95.76. The mean age of the participants was 28.33 (± 6.55 ± SD) years. Majority 33 (29.2 %) of the women were within the age group of 21-25 years followed by 26-30 which accounts 27 (23.0%). Almost all, 113 (99.1%), of the respondents were married at the time of the survey. 75 (66.4%) respondents were protestant in religion followed by catholic 32 (28.3%). Among the respondents, 75 (66.4%) were protestant followed by 32 (28.3%), catholic. Pertaining to educational status of the respondent, 33 (28.3%) of them had no formal education, 54 (47.8%) had primary education, while 23 (20.4%) and 4 (3.5%) had secondary and college educational status respectively [30]. Regarding occupation, 72 (63.7%) of the respondents were house wife, followed by 18 (15.9%) private employee, the rest 16 (14.2%), 7 (6.2%), of them were farmer and government employee respectively (Table 1).
| Socio-demographic characteristics | Frequency | Percentage | |
|---|---|---|---|
| Age | </=20 years | 12 | 10.6 |
| 21 years-25 years | 33 | 29.2 | |
| 26 yers-30 years | 27 | 23.9 | |
| 31 years-35 years | 22 | 19.5 | |
| >/= 36 years | 19 | 16.8 | |
| Total | 113 | 100 | |
| Religion | Protestant | 75 | 66.4 |
| Catholic | 32 | 28.3 | |
| Muslim | 3 | 2.7 | |
| Orthodox | 3 | 2.7 | |
| Total | 113 | 100 | |
| Occupation | House wife | 72 | 63.7 |
| Farmer | 16 | 14.2 | |
| Government employed | 7 | 6.2 | |
| Private employed | 18 | 15.9 | |
| Total | 113 | 100 | |
| Education | Can’t read and write | 11 | 9.7 |
| Read and write | 21 | 18.6 | |
| Primary | 54 | 47.8 | |
| Secondary | 23 | 20.4 | |
| College and above | 4 | 3.5 | |
| Total | 113 | 100 | |
| Marital status | Married | 112 | 99.1 |
| Single | 1 | 0.9 | |
| Total | 113 | 100 | |
Table 1. Socio-demographic characteristics of pregnant women who attend antenatal care at Pagak health center, South Sudan, N=113.
Reproductive history
Majority of the study subjects 73 (64.4%) of the women were multipara followed by 22 (19.5%), 12 (10.6%) and 6 (5.3%) were primipara, nullipara and grand multipara respectively. The mean parity (± SD) of the respondent was 2.67 (± 1.67). Pertaining abortion, about 21 (18.6%) had history of abortion in the past years [31,32]. Regarding ANC follow up during the current pregnancy those who had one visit, two visit, three visit and four visit were 35 (31.0%), 54 (47.8%), 19(16.8%) and 5(4.4%) respectively as depicted in Table 2.
| Reproductive history | Frequency | Percent | |
|---|---|---|---|
| Parity | Nulli para | 12 | 10.6 |
| Primipara | 22 | 19.5 | |
| Multi para | 73 | 64.6 | |
| Grand multipara | 6 | 5.3 | |
| Total | 113 | 100 | |
| Abortion | Yes | 21 | 18.6 |
| No | 92 | 81.4 | |
| Total | 113 | 100 | |
| ANC visit | One | 35 | 31 |
| Two | 54 | 47.8 | |
| Three | 19 | 16.8 | |
| Four | 5 | 4.4 | |
| Total | 113 | 100 | |
Table 2. Reproductive history of pregnant women who attend antenatal care at Pagak health center, South Sudan, N=113.
Knowledge of the respondent about mother to child transmission of HIV/AIDS and its prevention
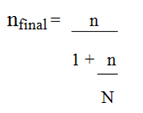
The study attempted to assess the knowledge of pregnant mothers attending ANC on MTCT of HIV. All pregnant enrolled in this study heard about HIV/AIDS but 23 (20.4%) of them didn’t heard about MTCT of HIV. Regarding the time of transmission of the virus from the infected mother to her child, those respondent who believed that he time for transmission during pregnancy, labor and obreast feeding were 14 (12.4%), 12 (10.6%) and 22 (19.5%) respectively. When these pregnant mothers asked about infant feeding option for a HIV+woman, majority, 90 (79.4%) cow milk is the best method, followed by 53 (46.9%), mixed feeding in the first 6 months of life and 40 (35.4%) exclusive breast feeding for the first 6 months as shown in Table 3. Generally, according to this study, 78 (69%) of the respondents have good knowledge about MTCT of HIV/AIDS as shown in Figure 2 [33-35].
| No. | Knowledge about PMTCT | Responses | Frequency | Percent |
|---|---|---|---|---|
| 1 | Heard about PMTCT | Yes | 90 | 79.6 |
| No | 23 | 20.4 | ||
| Total | 113 | 100 | ||
| 2 | Transmission during pregnancy | Agree | 14 | 12.4 |
| Disagree | 14 | 12.4 | ||
| Do not know | 85 | 75.2 | ||
| Total | 113 | 100 | ||
| 3 | Transmission during labor | Agree | 12 | 10.6 |
| Disagree | 25 | 22.1 | ||
| Do not know | 76 | 67.3 | ||
| Total | 113 | 100 | ||
| 4 | Transmission during breast feeding | Agree | 22 | 19.5 |
| Disagree | 12 | 10.6 | ||
| Do not know | 79 | 70 | ||
| Total | 113 | 100 | ||
| Infant feeding option for a HIV+woman | ||||
| 5 | Infant formula | Yes | 12 | 10.6 |
| 6 | Cow milk | Yes | 90 | 79.6 |
| 7 | Exclusive breast feeding for the first 6 months | Yes | 40 | 35.4 |
| 8 | Mixed feeding for the first 6 months | Yes | 53 | 46.9 |
Table 3. Knowledge of the respondent about mother to child transmission of HIV/AIDS and its prevention.
Figure 2: Knowledge about MTCT of HIV
Attitude of the respondent about mother to child transmission of HIV/AIDS and its prevention
Among 90 respondents who have heard about mother to child transmission, only 67 (74.4%) accepts the test result if it is positive, 34 (37.7%) could tell to their spouse if the test result is positive and 87 (94%) agreed to accept their spouse if test result will be positive. Pertaining to the screening, 74 (82.2 %) believe that pregnant women should be screened for HIV on Voluntary base. Pertaining to their preference of delivery birth attendant 74 (84.4%) of the respondent agreed that every woman must delivered by skilled person [36,37]. In this study some pregnant woman, 34 (37.7%), believed that No special treatment is need for HIV positive mothers during pregnancy. Nearly quarter, 22 (24.5%), of the respondents agree with the statement that woman opt to breastfeed despite HIV status as shown in Table 4. Generally, according to this study, 78 (69%) of the respondents have good attitude about MTCT of HIV/AIDS as shown on Figure 3.
| Attitude about PMTCT | Frequency | Percentage | ||
|---|---|---|---|---|
| 1 | What will you do if your test result is positive | Accept the result | 67 | 74.4 |
| Reject the result | 23 | 25.6 | ||
| Total | 90 | 100 | ||
| 2 | If you become HIV positive could tell your husband | Agree | 34 | 37.7 |
| Disagree | 56 | 62.3 | ||
| Total | 90 | 100 | ||
| 3 | What will you do if your spouse becomes tested result positive? | Support | 87 | 96.6 |
| Reject the result | 3 | 3.4 | ||
| Total | 90 | 100 | ||
| 4 | Pregnant women should be screened for HIV on Voluntary base | Agree | 74 | 82.2 |
| Disagree | 16 | 17.8 | ||
| Total | 90 | 100 | ||
| 5 | HIV infected pregnant mother must delivered with skilled person | Agree | 76 | 84.4 |
| Disagree | 14 | 15.6 | ||
| Total | 90 | 100 | ||
| 6 | No special treatment is need for HIV positive mothers during pregnancy | Agree | 56 | 62.3 |
| Disagree | 34 | 37.7 | ||
| Total | 90 | 100 | ||
| 7 | HIV positive women should breastfeed despite HIV status due to stigma | Agree | 22 | 24.5 |
| Disagree | 68 | 75.5 | ||
| Total | 90 | 100 | ||
Table 4. Attitude of the pregnant women about mother to child transmission of HIV/AIDS and its prevention.

Figure 3: Attitude of pregnant women towards MTCT.
Practice about PMTCT
Prevention of mother to child transmission among women was assessed using different explanatory variables. About threefourth of the respondents have been tested for HIV. Among the tested all had pre and post-counseling services and discussed with their husband about HIV testing Among the respondents, 63 (74.1%) shared the result of HIV test with their husband/partner as depicted in Table 5.
| Practice about PMTCT | Responses | Frequency | Percentage | |
|---|---|---|---|---|
| 1 | Have you tested for HIV? | Yes | 85 | 75.2 |
| No | 28 | 24.8 | ||
| Total | 113 | 100 | ||
| 2 | Have you discussed about HIV testing with your partner/ boyfriend/husband? | Yes | 85 | 75.2 |
| No | 28 | 24.8 | ||
| Total | 113 | 100 | ||
| 3 | Did you receive any pre-test counseling before you undertook your HIV test? | Yes | 85 | 75.2 |
| No | 28 | 24.8 | ||
| Total | 113 | 100 | ||
| 4 | Did you receive any post-test counseling when you got your HIV test result? | Yes | 85 | 75.2 |
| No | 28 | 24.8 | ||
| Total | 113 | 100 | ||
| 5 | Sharing test result with husband | Yes | 81 | 71.1 |
| No | 32 | 28.9 | ||
| Total | 113 | 100 | ||
Table 5. Practice of pregnant women about PMTCT.
Factors associated with knowledge of the pregnant mothers about PMTCT
Bivariate and multivariate analysis was performed between Knowledge about MTCT (dependent variable) and each independent variable. Binary logistic regression was performed to assess the association of each independent variable with Knowledge of pregnant women about MTCT. The factors that showed a pvalue of 0.2 and less were added to multivariate regression model.
Among the variables that were included in the multivariate analysis model mother’s education an number of ANC visit were significantly associated with knowledge about MTCT of HIV
Factors associated with knowledge of the pregnant mothers about PMTCT
Bivariate and multivariate analysis was performed between knowledge about MTCT (dependent variable) and each independent variable. Binary logistic regression was performed to assess the association of each independent variable with Knowledge of pregnant women about MTCT. The factors that showed a p-value of 0.2 and less were added to multivariate regression model.
Among the variables that were included in the multivariate analysis model mother’s education an number of ANC visit were significantly associated with knowledge about MTCT of HIV.
Pregnant women whose educational status is secondary and above had four times knowledge about MTCT than their counter party (AOR=4.50: 95% CI (1.18-17.07)). Pertaining ANC visit, pregnant women who had repeated visit had three fold knowledge about MTCT than their counterpart (AOR=3.58: 95% CI (1.49-8.60)) as shown in the Table 6.
| S. No | Variables | Knowledge about MTCT | COR | AOR | P-value | ||
|---|---|---|---|---|---|---|---|
| Good | Poor | ||||||
| 1 | ANC visit | Repeat visit | 55 | 14 | 3.58 (1.55-8.25) | 3.58 (1.49-8.60) | 0.004 |
| First visit | 23 | 21 | 1 | ||||
| 2 | Mothers education | Secondary and above | 24 | 3 | 4.74 (2.7-27.5) | 4.50 (1.18-17.07) | 0.027 |
| </= primary level | 54 | 32 | 1 | 1 | |||
| 3 | Gravidity | Multi gravida | 73 | 28 | 3.65 (1.07-12.46) | 3.01 (0.82-10.98) | 0.094 |
| Primi gravida | 5 | 7 | 1 | 1 | |||
Table 6. Factors associated with knowledge of the pregnant mothers about PMTCT.
The study found that, 79.6% of the respondent heard about mother to her child transmission of HIV. This finding is in line with a study conducted in Southern Ethiopia, where 75.3% knew that HIV can be transmitted from infected mother to her child. In this study, the overall good knowledge and attitude towards mother to child transmission of HIV was 63% and this finding is in line with the study done in Mizan Tepi which accounts for 65.9%.
Pertaining the time of transmission, 12.2% responded during pregnancy, 10.6% transmission during labor and 19.6% during breast feeding. This finding is very low in knowledge when comparing with study conducted in Southern Ethiopia where 100 (58.8%) said during pregnancy, and 80 (47.1%) replied during labor and delivery, 115 (67.6%) replied during breastfeeding while 51 (30%) do not know the time of transmission. The likely reason for this discrepancy could be Pagak has in war for many years.
In this study practice towards prevention of mother to child transmission among women was assessed and about three-fourth of the respondents have been tested for HIV. Among 71 (78.8%) had discussion with their husband about HIV testing. Among the tested all had pre-and post-counseling services. Among the respondents, 63 (74.1%) shared the result of HIV test with their husband/partner. This finding is comparable with result of Hawassa and a study conducted in Mizan tepi.
Generally, according to this study, 78 (69%) of the respondents have positive attitude about MTCT of HIV/AIDS and this finding is a bit lower than the study conducted in Mzan Tepi which is (75.9%), Ambo hospital were 221 (93.6%) have positive attitude and the study done Hawassa university referral hospital which have showed that 97.4% had good attitude towards it. However, a bit higher than study done in south Sudan juba, where only half of the pregnant women (51%) showed positive attitudes toward PMTCT measures.
Among 90 respondents who have heard about mother to child transmission, only 34 (37.7%) could tell to their spouse if the test result is positive. This finding is lower than a study done in west Ethiopia which has showed that 71.6% of the pregnant women could tell to their spouse if the test result is positive. Pertaining to the preference of birth attendants 74 (84.4%) of the respondent agreed that every woman must delivered by skilled person. Again this result is in line with the study done in Ambo which has showed 91% agreed that every woman must delivered by skilled person.
Pregnant women whose educational status are secondary and above have had four times knowledgeable than their counter part on PMTCT (AOR=4.50: 95% CI (1.18-17.07)). That is to say the more the level of education, the more the knowledge on MTCT and the less the education, the less the knowledge on PMTCT. Pertaining ANC contacts, pregnant women who had repeated contacts had three fold knowledgeable on PMTCT than their counterpart (AOR=3.58: 95% CI (1.49-8.60)). This finding is in line with the studies conducted in Ambo and southwest Ethiopia (Benchmaji) 29, 31 respectively.
This study concluded that educational status and numbers of ANC contacts are crucial for the knowledge, attitude and practice on PMTCT. Moreover, the study explored that the pregnant women had moderate knowledge, attitude, and practice as we compared to the similar study conducted in the neighbor’s countries.
Ethical approval was obtained from the research and publications committee of department of gobal health, college of health science, and Addis Ababa university. A formal letter for permission and support was written to ministry of health of South Sudan, upper Nile state, and Maban county. Similarly, Consent from the Pagak health center was obtained prior to commencement of the study. The purpose of the study was clearly explained to concerned bodies. All the study participants were informed the purpose of the study, their right to completely free to choose whether or not to participate, and so written as well as verbal consent was also obtained from respondents. Confidentiality was maintained and assured by excluding their names from identification of the study subjects.
• Intervention and improvement are much needed to extend the
PMTCT services to larger scale.
• Girls education is more important as to understand PMTCT and
result in to good health of both mother and baby.
• Increasing male involvement is important in PMTCT.
• Farther study needs to be conducted not only in pagak but also
in entire south Sudan.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Michael Pou Machar. "Assessment of Knowledge, Attitude, Practice of Mother to Child Transmission of HIV (MTCT) among Pregnant Mothers Attending Antenatal Clinic at Pagak Health Center, South Sudan". J HIV AIDS Res, 2023, 5(1), 1-11.
Received: 13-Mar-2023, Manuscript No. JHAR-23-91520; Editor assigned: 15-Mar-2023, Pre QC No. JHAR-23-91520 (PQ); Reviewed: 29-Mar-2023, QC No. JHAR-23-91520; Revised: 05-Jun-2023, Manuscript No. JHAR-23-91520 (R); Published: 12-Jun-2023, DOI: 10.35248/JHAR.23.5(1).001
Copyright: © 2023 Machar MP. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.