Case Report - (2024) Volume 5, Issue 2
Orthodontics and periodontics have a strong co-relation especially when treatment of periodontally weak dentition is considered. This holds even more importance when orthodontic treatment is carried out on adult patients. Many authors have studied the deleterious effects of orthodontic treatment on the periodontium but this article focuses on how conservative orthodontic treatment helps in improvement of the health of the periodontium as well as harmonises the attrided dentition. The article presents a case of generalised aggressive juvenile periodontitis with tongue thrust habit and interdental spacing treated with a habit breaking appliance.
Orthodontics involves optimum force application to facilitate movement of teeth in desired direction. The same principle is applied here wherein the deleterious forces due to improper tongue posture are eliminated while the tongue is guided in its proper place which in turn facilitates interdental space closure. As the treatment is conservative of any extra forces from the labial side of teeth, it is seen that the health of the periodontium is improved and the traumatic occlusion is taken care of.
Periodontium • Traumatic • Malocclusion • Thumb sucking • Tongue thrusting
Dental malocclusion is known to originate from a number of etiological factors, including parafunctional habits. The two most prevalent oral behaviors are thumb sucking and tongue thrusting.
Tongue thrust is a defined as a condition in which the tongue makes contact with any teeth anterior to the molars during swallowing. Tulley states tongue thrust as the forward movement of the tongue tip between the teeth to meet the lower lip during deglutition and in sounds of speech, so that the tongue becomes interdental.
Tongue thrust can be primary, the etiological factors of which include learned behavior, hyperplastic tonsils, prolonged thumb sucking, nasal congestion and macroglossia, or can be secondary to early extraction of deciduous teeth or an anterior open bite.
An infantile swallowing behaviour that continues until late childhood is known as tongue thrust. Breathing and speech problems, an open bite, and teeth that protrude are the results of this. Most kids effectively change their swallowing habit during during their formative years, going from an infantile to a mature one. However, some people retain their infancy habits of swallowing and tongue thrusting, which may be caused by an unhealthy habit like thumb sucking or an underlying condition like swollen adenoids. By early discovery and intervention in a developing youngster, the impacts of these practises can be averted. Treatment options for tongue thrust include early detection, eradicating underlying causes, adjusting tongue posture, and breaking bad habits with orthodontic appliances. Several oral myofunctional therapy procedures are used to correct tongue problems.
When pressures that keep teeth in their natural position in relation to their arch are disrupted, it results in pathologic migration, which is defined as shift in tooth position. Several causative causes may contribute to the disturbance of tooth position balance. These include predisposing and external factors such as bone loss, tooth loss, gingival inflammation, age, parafunctions, lingual interposition in the tongue thrust, and oral habits [1].
Various systemic conditions also lead to or have an additive effect on variable degrees of periodontitis and these are of utmost importance when juvenile aggressive periodontitis is seen.
According to Jepson, et al. in 2017, Diabetes should be acknowledged as an essential modifying factor and included in a clinical diagnosis of periodontitis as a descriptor rather than being viewed as a separate diagnosis for diabetes associated periodontitis.
Treatment options for these behaviours include eliminating the etiology, retraining exercises, and the use of mechanical restraints. In order to break the practice of tongue thrusting, tongue crib tools are incredibly helpful. The tongue cannot protrude mechanically between the incisors thanks to this mechanical barrier.
Profit contends that rather than tongue pressure during thrusting, the anterior tongue position at rest may have a bigger influence on tooth position [2]. Therefore, the main goal of the treatment is to teach the tongue to remain in its natural position above the teeth. The first and most crucial stage in the treatment of the tongue thrusting habit is the elimination of the etiology. Once the root cause has been identified and eliminated, there are typically two ways to treat the habit of thrusting the tongue forward:
• Mechanical restraining, which involves placing an
appliance in the mouth to prevent tongue thrusting forward.
• Muscle retraining, which involves an exercise technique
to re-educate the muscles involved in swallowing.
Clinical findings and diagnosis
A 23 years old, female patient reported to the department of orthodontics and dentofacial orthopaedics with the chief complaint of spacing in between the teeth. The patient reported no abnormal medical history. On asking for the dental history, she reported frequent bleeding from gums and had under periodontal treatment in the form of sub-gingival scaling in the past 3 months-4 months [3].
She also reported a familial history of diabetes with swollen and receding gums.
On extra oral examination, she had a symmetrical face with a straight profile, competent lips and a consonant smile arc on smiling. On smiling, the patient showed 50%-60% display of the maxillary teeth.
Intra-oral examination revealed an angle’s class I molar relation and a class I canine relation bilaterally. There was reduced over jet and overbite with incisors in an edge to edge relation. Moderate interdental spacing was noted. There was generalised attrition of the entire dentition suggestive of a bruxism habit or traumatic occlusion. Patient did not report of any bruxism habit on further interrogation. There was bleeding on probing from gums as well as mild recession of gums. Patient had undergone periodontal treatment in the form go sub gingival scaling and curettage recently.
On clinical functional examination, the patient had an anterior tongue thrust habit which was corroborating with the increasing interdental spacing with time.
The evident findings noted on the OPG were mild generalised horizontal bone loss, missing 28, 38 and 48 and a root canal treated (Figure 1) [4].
The lateral cephalogram Figure 2 showed a well-balanced skeletal and soft tissue profile with proclined anterior teeth.
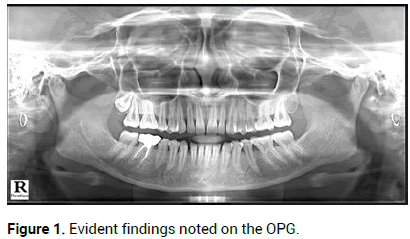
Figure 1: Evident findings noted on the OPG.
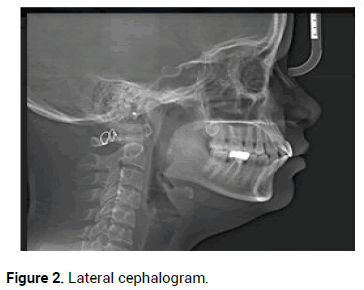
Figure 2: Lateral cephalogram.
Treatment plans
• Habit correction for tongue thrusting followed by fixed
orthodontic appliance for interdental space closure.
• Patient was informed about the nature of problem and the
retention protocol that will be required post-orthodontic
treatment.
Treatment progress
The initial pre-treatment records were taken. Followed by that, fixed tongue crib that was soldered to the molar bands was cemented on the first molars. Patient was very well counselled for the need of the tongue cribs and accepted to wear the appliance. A one week follow-up was taken to assess the changed swallowing pattern of the patient and adaptation to the new appliance. As habit correction was the main objective, bonding of fixed appliance was fdelayed. In about two months of wear of the appliance, the patient started noticing the gradual decrease in interdental spacing. This was observed as the spacing was mainly due to the excessive tongue pressure which had disturbed the pressure balance. Seeing the positive change without any additional application of forces, patient later on refused to wear the fixed orthodontic appliance [5]. Therefore, as the main etiology of the problem was addressed and solved, the treatment ended with fixed lingual retainers in place. Addressing the root cause of the problem ensured long term stability of the treatment (Figures 3-5).
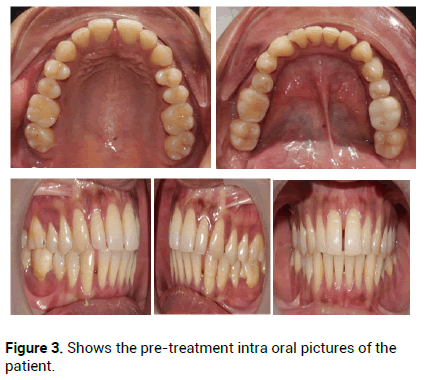
Figure 3: Shows the pre-treatment intra oral pictures of the patient.
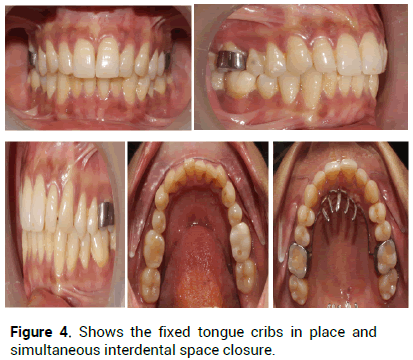
Figure 4: Shows the fixed tongue cribs in place and simultaneous interdental space closure.
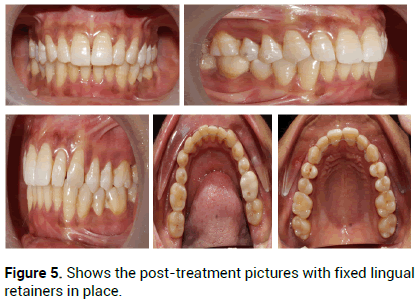
Figure 5: Shows the post-treatment pictures with fixed lingual retainers in place.
Treatment results
The interdental spaces have been completely closed without any complex biomechanics and inadvertent force application. A parallel marked improvement in the health of the periodontium was evident. An optimum positive over jet and overbite has been achieved. This has also relieved the attrition of anterior teeth due to an earlier edge to edge bite. Therefore, the patient has been relieved from the traumatic occlusion. The tongue has been trained for proper positioning with the elimination of tongue thrust habit. Fixed lingual bonded retainers are given as a part of retention protocol [6].
The new positions of the teeth have been stabilized by the fixed lingual bonded retainers to aid in reorganisation of the gingival and periodontal fibers. Thus, preventing the relapse of the treatment.
A yearlong follow-up of the patient is taken and no relapse has been seen with proper tongue resting position achieved [7].
After thorough examination of the patient, two key points were pointed out. First was the tongue thrust habit which had disturbed the orofacial muscular balance by applying inadvertent pressure from the palatal and lingual sides of incisors resulting into increasing interdental spaces. The pathologic migration of teeth was compounded by another factor which was the generalised mild horizontal bone loss suggestive of aggressive juvenile periodontitis which may be in its preliminary phase. The patient had reported a familial history of diabetes mellitus [8].
Successful orthodontic treatment necessitates thorough assessment and planning. Oral habits are just one of several environmental factors that might contribute to dental malocclusion. The frequency, persistence, and intensity of an oral habit affect how severe a malocclusion it causes. These behaviours change the dental arch and occlusal characteristics by interfering with muscle balance and bone growth. Therefore, it's crucial to identify behaviours and change them when necessary in order to prevent these negative impacts [9].
Tongue-thrust swallowing is described as the forward positioning of the tongue tip between the incisors during deglutition. When swallowing, tongue thrusting is a behaviour in which the tongue contacts any teeth before the molars. The most important step in stopping tongue pushing is to alter the tongue's natural resting position. To address tongue thrust, an orthodontist may utilise prongs, spikes, or other tongue reminders that correct the tongue rest position and swallow. The technique described in this article is efficient at repositioning the tongue while causing the patient the least amount of discomfort [10].
Abnormal tongue position in the context of increasing interdental spacing combined with horizontal alveolar bone loss must be evaluated and corrected with care. Before using habit breaking appliances, it is advised to begin with the least intrusive approaches, such as therapy and counselling. Correction of tongue thrusting is important for avoiding malocclusions it may cause. Redirecting tongue position with method used in this case report is effective in correcting tongue thrusting in adults with no inadvertent application of forces and a cost effective approach.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Maniyar V. "Conservative Orthodontic Treatment of a Periodontally Weak Spaced Dentition with Tongue Posture Correction- A Case Report". J Gen Dent, 2024, 5(2), 1-3.
Received: 21-Dec-2022, Manuscript No. JGD-22-84323; Editor assigned: 23-Dec-2022, Pre QC No. JGD-22-84323 (PQ); Reviewed: 06-Jan-2023, QC No. JGD-22-84323; Revised: 14-Mar-2024, Manuscript No. JGD-22-84323 (R); Published: 21-Mar-2024, DOI: 10.35248/dentistry.5.2.1-3
Copyright: © 2024 Maniyar V. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.