Mini Review - (2024) Volume 13, Issue 3
Mother's own milk is the best gift for fragile preterm newborns in terms of growth, nutrition and development. Most of the time this tiny babies deprived of mother's own milk because of delayed and infrequent expressions of breast milk. Parents of preterm babies often not aware of the benefits of preterm milk. In this article we discussed about the factors responsible for less availability of mother's own milk in Neonatal Intensive Care Unit (NICU) and various ways to overcome it.
Each year about 15 million babies worldwide are born prematurely, that is about 1 in 10 children. Out of 3 million children born every year in Bangladesh some 0.6 million are born premature, and out of that 0.6 million premature births 20,000 infants die [1]. Premature neonates face feeding challenges due to their immature GIT system, poor sucking and swallowing coordination, delay in starting feed due to morbidities leading to postnatal growth and nutritional failure. Human milk is beneficial for preterm babies, which comprises of mother’s own milk and pasteurized donor human milk [2,3]. Preterm and very low birth weight babies are at greatest risk of not receiving their own mother’s own milk due to critical condition of mothers. Donor human milk is recommended when mother’s own milk isn’t available. Mothers who separated from their babies face challenges to initiate and maintain breast milk expression and they require support from health care professionals from the very beginning. Mother’s own milk protects premature newborn from the leading causes of neonatal mortality like sepsis, NEC and other preterm birth related complications [4-6]. In the long term, mother’s own milk optimizes nutrition, growth and neurodevelopmental outcome, decrease Bronchopulmonary dysplasia (BPD), Retinopathy of prematurity (ROP), metabolic syndromes, inflammatory and atopic diseases [7,8].
Positive relationship was seen between the quantity of breast milk received during hospitalization and neuro developmental outcome in premature infants [9]. Mothers of the neonates admitted in NICU face biological difficulties, stress related to NICU admission and multiple challenges in establishing and maintaining an adequate supply of milk [10,11].
Significant delay and less availability of mother’s own milk is noted due to lack of proper communication, counseling, and lactation support. It’s a real challenge for health care team to overcome this constraint. Early and sustained availability of mother’s own milk will not only decrease over all morbidity and mortality but may also ensure adequate weight gain to prevent extra uterine growth retardation and lesser duration of hospitalization [12]. It’s known that premature breast milk contain more protein, fats, calories and antibodies than mature milk to meet the need of a premature baby and most of the time this shared breast milk is mature milk that is not tolerated by the premature gut [13].
WHO recommendation (2022)
WHO recommended mother’s own milk feeding for preterm or Low- Birth-Weight (LBW) babies, including very preterm (<32 weeks’ gestation) or very LBW (<1.5 kg) babies.
When mother’s own milk is not available, donor human milk may be considered for feeding of preterm or Low-Birth-Weight (LBW) babies, including very preterm (<32 weeks’ gestation) or very LBW (<1.5 kg) babies.
Difference between composition of preterm and term breast milk
Milk from women who deliver prematurely differs from that of women who deliver at term. Preterm milk is initially higher in protein, fat, Glycosaminoglycan (GAG), free amino acids, bioactive molecules [14]. Glycosaminoglycan act as decoy providing binding sites for pathogenic bacteria to prevent adherence to the enterocyte. Premature milk is richer in GAG than term milk [15]. Lactose is low in colostrum, and it increases over time with more increases in preterm milk. Another important carbohydrate of human milk is complex oligosaccharides. Human Milk Oligosaccharides (HMOs) are not digested by host glycosidase and produced in large amounts in human milk. Its structure is highly variable among mothers [16]. Functions of HMO are: Prebiotic, that stimulate the commensal bacteria containing the bacterial glycosidase to deconstruct and consume the HMOs, [17], decoy HMO has structural similarity to the glycan on enterocytes allows it to competitively bind to pathogens [18], and fructose and sialic acid component of HMO play important role in host defense and neurodevelopment respectively [19]. Human milk oligosaccharides content is highly variable in preterm milk. This difference is due to genetic diversity [20]. Fucosylated content of HMOs is also variable in mothers delivering preterm babies (Figure 1) [21].
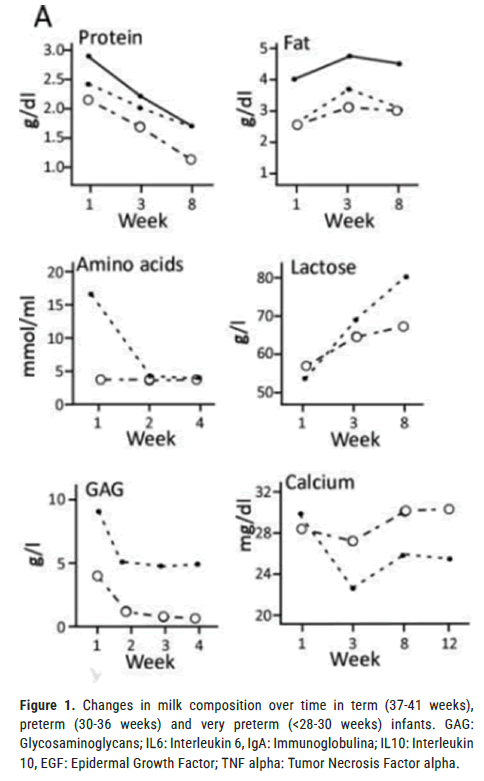
Figure 1. Changes in milk composition over time in term (37-41 weeks),
preterm (30-36 weeks) and very preterm (<28-30 weeks) infants. GAG:
Glycosaminoglycans; IL6: Interleukin 6, IgA: Immunoglobulina; IL10: Interleukin
10, EGF: Epidermal Growth Factor; TNF alpha: Tumor Necrosis Factor alpha. 
Challenges of providing mother’s own milk to premature infants: Although mother’s own milk is best for preterm and low birth weight newborns often this preterm babies are deprived of mother’s own milk in the first few days of life [22]. Studies show that various factors are responsible for failure of expression within one hour of birth. Among these factors, mode of delivery, educational status of the mother, poor latching significantly affects early initiation of breast milk expression within one hour of birth [23].
Studies showed the following factors responsible for less mother’s own milk supply:
• Inadequate knowledge regarding the advantage of mother’s own milk among the mothers
• Delayed expression of milk
• Insufficient milk volume
• Decreased frequency of breast milk expression
• Lack of proper knowledge regarding procedure of expression
• Lack of counseling protocol in neonatal unit.
• Separation of mother and baby due to NICU admission
• Lack of privacy to express breast milk.
• No hospital policy for early expression of breast milk for preterm baby
• Maternal health issues
• Problems of breast like sore nipple, engorgement, mastitis, etc.
• Unavailability of proper breast pump like hospital grade electronic breast pump.
• Lack of family support
Intervention to increase the quantity of expressed milk for preterm baby
Preterm babies are unable to feed directly at the breast due to immature sucking, swallowing coordination. Mothers of preterm babies require lactation support just after birth to express colostrum which is rich in bioactive molecules. Early expression of breast milk will maintain milk output to facilitate direct breast feeding and exclusive mother’s own milk feeding at discharge [24].
Intervention helping in increasing quantity of expressed milk.
Comprehensive counselling Package: Counseling during antenatal period, during admission in NICU and throughout the hospital stay to mother and care giver regarding.
• Importance of mother's own milk for preterm baby
• Difference between preterm and term milk.
• Importance of early initiation breast milk expression within 6 hours of birth, preferably within one hour.
• Increasing the frequency of breast milk expression (2hrly).
• Expression of breast milk at night
Demonstration of breast milk expression
Milk can be expressed by hand and breast pump. Both methods should be demonstrated to mother to ensure early and frequent expression of breast milk. Practical demonstration can be done by using dummy breast as well as on mother’s breast video and pictorial demonstration of milk expression is useful for mother and caregivers.
Early expression of breast milk: Mothers need support for milk expression within the first one to three hours after delivery or as soon as possible (Baby friendly Hospital Initiative for small, sick and preterm newborns, 2020). With early expression of breast milk preterm baby will get the benefits of colostrum. The first milk or “colostrum” termed as liquid gold which is rich in protective factors. Lactogenesis â?¡ is often delayed in mothers who deliver preterm babies due to delayed and infrequent expression of breast milk. Studies show that lactogenesis â?¡ can be achieved in due time by early (within 1-3 hr) and frequent (2 hrly) expression of breast milk. This ensures increase duration of lactation and hence prevents lactation failure [25].
Frequent (2 hrly) expression of breast milk: As the preterm babies with gestational age less than 34 weeks have poor sucking and swallowing coordination so expressing breast milk at a regular interval will increase and maintain mother’s milk flow. Two hourly expression of breast milk leads to stimuli for more milk production and hence maintaining lactation. It is recommended to express breast milk at least 8 times per day because less frequent expression of breast milk at this stage may limit maximum milk production [26,27].
Night time expression of breast milk: Night time expression is important for hormonal stimulation and continued milk production. Prolactin is produced more at night, so night time expression of breast milk is helpful for maintaining the milk supply. Mothers should express milk 2 hrly at night with a 4 hrs gap to ensure rest. They can express breast milk at 12 am, take an uninterrupted sleep for 4hrs then again express milk on waking up.
Various methods of milk expression: Breast milk should be expressed manually by hand during first 2 days as colostrum is thick and small in amount. From day 3 onwards breast milk can be expressed by manual and electric breast pump. Milk volume is more with hospital grade electric breast pump than manual breast pump.
Technique of breast milk expression: Proper technique of breast milk expression not only ensures adequate amount of milk for baby but also prevent complications related to improper technique of breast milk expression like sore nipple, breast engorgement [28]. Use of proper flange of breast pump, proper sealing and proper pressure needed for timely adequate amount of milk expression.
Kangaroo Mother Care (KMC): Early KMC in preterm neonates reduces time to full feeds (150 ml/kg/day). It increases the availability of mother’s own milk and results in better weight gain [29].
Breast milk expression chart/pumping diary: Studies have shown that maintaining a breast milk expression chart/pumping diary can find out the time when breast milk expression is less as well as the volume of breast milk can be ascertained. This timely breast milk expression according to chart leads to significant increase in the milk volume and intake of mother’s own milk among the preterm neonates admitted in NICU. Phycians and nurses should check the bed side breast milk expression chart/breast milk pumping diary to find out the pitfall and solution of it. They can praise the mother on regular timely breast milk expression based on the chart or pump dairy. This ensures sustainability in breast milk expression. Exclusive mother’s own milk feeding significantly reduces the time to reach the full enteral feeding and ensure early discharge from hospital. The breast milk pumping diary help through positive feedback mechanism [30].
Support of skilled professional, peer support: Evidence suggests that both health care professionals and peer support for mothers contribute to the success of breast feeding in babies. Literature also proposes a positive effect of education and lactation support on maternal decision to provide exclusive mother's own milk for very low birth weight infants.
Support of family: Mothers of preterm babies most of the time delivered by Lower Uterine Segment Cesarean Section (LUCS) due to preterm birth related complications. Moreover, fear of Neonatal Intensive Care Unit (NICU) admission, separation from the baby lead to mental stress, anxiety and worries. Together this physical and mental stress causes less milk production. So other members of family should give support to her regarding breast milk expression and involve her in family cantered care.
Provision of M-SCANU: Separation from baby and maternal mental stress responsible for less mother’s own milk availability. M-SCANU will facilitate 24 hrs rooming in with baby that will decreases mother’s anxiety, stress, ensure uninterrupted Kangaroo Mother Care (KMC) and thereby early and frequent expression of breast milk.
Family cantered care: Implementation of family integrated care increases breastfeeding rates of preterm infants at discharge, and it can really support breastfeeding of preterm infants [31].
Oral care with colostrum: Even if the preterm baby kept NPO for 24- 48 hrs, mother should express breast milk to give oral care. This not only gives immunoprotective effect but also ensures continuity of breast milk expression and thereby increasing the milk volume. Various morbidities related o preterm birth can be reduced by oropharyngeal administration of colostrum like late-onset neonatal sepsis, NEC, Disseminated Intravascular coagulation (DIC), use of MV and inotropes, duration of inotropes in preterm infant [32].
Non-Nutritive Sucking (NNS), breast warming, and breast massage, music relaxation therapy: These techniques can be used before breast milk expression to relieve breast engorgement, increase blood flow to breast and stimuli for breast milk production
Exclusive mother's own milk fed preterm neonates have better short term outcomes, early discharge and better long term neurodevelopmental outcomes. Unfortunately, prematurity raises barriers for the initiation of mother’s own milk feeding and its continuation. Support to mother as well as to whole family from antenatal period up to discharge will optimize mother’s own milk supply for preterm baby in Neonatal Intensive Care Unit (NICU). Improvement in early and frequent expression of breast milk leads to increase in volume of expressed breast milk and exclusive mother's own milk feeding among the preterm neonates throughout the hospital stay and at discharge.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this ar ticle.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Afreen S, et al. Mother’s Own Milk for Preterm Neonates: Barriers and Ways to Overcome it. J Biol Todays World, 2024,13(3), 001-004
Received: 16-May-2024, Manuscript No. JBTW-24-135625; Editor assigned: 20-May-2024, Pre QC No. JBTW-24-135625 (PQ); Reviewed: 03-Jun-2024, QC No. JBTW-24-135625; Revised: 10-Jun-2024, Manuscript No. JBTW-24-135625 (R); Published: 17-Jun-2024, DOI: 10.35248/2322-3308-13.3.001
Copyright: © 2024 Afreen S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited