Research Article - (2021) Volume 10, Issue 6
Background: Up to the 21st century, Traditional, Complementary and Alternative Medicine (TCAM) is still used despite the wide spread of orthodox medicine. The magnitude, predictors and types of herbal remedies used for COVID-19 are assessed to tailor evidence based policy and drug formulation against COVID-19.
Methods: A community based cross sectional study was conducted among 1100 respondents from nine (9) communities selected in three health districts from May to July 2020. Pretested structured questionnaires were used to collect data from selected households on the use of TCAM, predictors as well as on the herbal preparations used for COVID-19. Nineteen (19) traditional healers were also interviewed on the types of herbal preparations use on patients tested or suspected for COVID-19 and the signs and symptoms observed. P-value <0.05 were considered to be statistically significant in multivariate logistic regression analysis. Atlas ti V 7.5 was used for types of herbal species reported.
Results: Of the 1100 participants sampled, 754 (68.5%) had used TCAM in the last 12 months, 95%CI: 66.3-71.5. A total of 24.4% (95%CI: 20.6-29.1) of the participants used herbal remedies for COVID-19. Allium sativum, Azadirachta indica, Zingiber oficinale, Artemisia annuawere most commonly used herb for COVID-19. Cough, catarrh and fever were the main symptoms of COVID-19. Herbalists 79.7% (95% CI: 77.3-82.1) and bone setters 14.9% (95% CI: 12.8-17.0) were mostly visited. Logistic regression analysis showed age >41 years (95% CI: 1.09-4.91), being a farmer (95% CI: 1.99-5.34), income levels between 185-370 USD (95% CI: 1.33-4.55), participants who resided in a rural setting (95% CI: 1.04-3.98), being knowledgeable on TCAM (95% CI: 1.54-6.45) and having a positive attitude towards TCAM (95% CI:1.94-6.45) were predictors for TCAM use.
Conclusion: TCAM is widely used even in the era of orthodox medicine, and many factors contribute to its use in the Southwest Region of Cameroon which should be taken into consideration in healthcare interventions that are sensitive to TCAM. Herbal preparations used during the COVID-19 pandemic can serve as baseline for drug development through efficacy and toxicity tests.
Prevalence • Predictors • TCAM • COVID-19
TCAM: Traditional, Complementary and Alternative Medicine; TM: Traditional Medicine; COVID-19: Coronavirus Disease 2019; THP: Traditional Health Practitioners; OHPs: Orthodox Health Practitioners; OM: Orthodox Medicine; WHO: World Health Organization; UHC: Universal Health Coverage; SSA: Sub-Saharan Africa.
Traditional, Complementary and Alternative Medicine (TCAM) are a group of healthcare practices (indigenous or imported) that are delivered outside of the mainstream healthcare system [1]. In the African context TCAM may include the use of local herbal medicines or products, indigenous healthcare practices (such as traditional bone setting, traditional birth attendants), as well as imported complementary and alternative medicine products and practices (eg, acupuncture or chiropractic) [2]. According to the world health organization, TCAM can contribute to improving quality of healthcare services through integration, regulation of TCAM products/ services used by communities, strengthening sustainability and resilience through maximizing potentials of TCAM [3]. WHO estimates that more than 80% of the African populations rely on traditional medicine for their healthcare needs [4]. A systematic survey from 32 countries from non- Sub-Saharan Africa region shows a TCAM provider use prevalence of 34.7% in Australia, in Europe ranging from under 10% in Bulgaria, Poland and Slovenia to 35.4% in France, in Asia from 16.7% in Russia, to over 50% in China mainland, the Philippines and Republic of Korea, and over 20% in the USA, Chile and South Africa [5]. A recent systematic survey conducted in SSA shows traditional, complementary and alternative medicine use in the general population, reporting substantial prevalence ranging from 4.6% (urban settlement in Ethiopia) to 94% (semi urban settlements in Nigeria and Ethiopia), with an estimated average of 58.2% [6]. Various prevalence was also observed among 10 articles that reported on TCAM practitioner utilization (1.2%-67% (mean, 28.8%)) across four identified studies with smaller sample sizes. The with higher prevalence reported in Tanzania (77.1%) [6]. Reports from world health organization show TCAM use in Uganda and Tanzania at 60%, in Benin and Rwanda at 70%, and in Ethiopia at 90% [6].
In low-and middle-income countries, TCAM use has been associated with lower educational and socio-economic status [7,8], relative low cost and flexibility of payment of TCAM products and services, accessibility, perception of TCAM being natural and therefore safe as well as effective compared with orthodox healthcare. In another study patient’s trust and confidence in their traditional medicine practitioners were factors associated with TCAM product and practitioner use [6].
Unsurprisingly, there has been an uptick in the amount of research being conducted at the intersection of TCAM and COVID-19 [9]. Several doctors and researchers have already attempted to use herbal medicines on clinical trials against SARS-CoV-2 [9].The longstanding use of dietary therapy and herbal medicine to prevent and treat diseases cannot be overemphasized, as several herbs exhibit antiviral activity [10]. Types of herbal medicine to prevent SARS-CoV-2 infections could serve as a baseline for drugs development [11].
Recently the Madagascar Institute of Applied research linked the use of Artemisia annua (sweet wormwood) in COVID-19 [11]. Zimbabwean government was reported to have authorized herbalists to treat patients with COVID-19 symptoms raising concerns among national public health experts [9]. There is a lack of adequate data on the use of TCAM during the COVID-19 pandemic in Africa and in Cameroon in particular.
There is dearth of research and data from Cameroon on the extend and predictors of TCAM use, as well as types of herbal preparations use in the general population for COVID-19 which is very necessary for policy formulation/population based healthcare interventions that are sensitive to TCAM, regulation and further research on the efficacy and toxicity of these herbals use for COVID-19.
Study area
Cameroon has about 90% of the African ecosystems which includes; the Sahelian, Sudan, humid tropical forest, afro mountains, coastal and mountain eco-regions [12]. This study was conducted in the Fako Division in the Southwest Region of Cameroon. Fako Division lies in the coastal region between 4°28´30″N and 3°54´26″N latitudes, and 8°57´10″E and 9°30´49″ E longitudes. The land area is approximately 203,071.27 ha and has a population of 534854 people. Most inhabitants practice agriculture as the main economic activity [12]. The region has two seasons: the dry season from October to March and the wet season from April to September. Almost all ethnic groups in Cameroon are represented in the region, attracted by the fertile volcanic soil for agriculture. The study was conducted in nine (9) communities (Isokolo-Limbe, Mile 4-Limbe, Down Beach-Limbe, Buea town, Muea-Buea, Mile 16-Buea, Likumba-Tiko, Water tank-Tiko (Camp) and Small Ekange-Tiko (Camp) i.e 3 communities selected from the Buea, Tiko, and Limbe Health Districts in the Southwest Region of Cameroon.
Study design
This was a cross-sectional survey conducted in 9 communities in the South west region Cameroon. Nine communities were selected within the 3 health districts and semi-structured questionnaires administered to examine traditional, complementary and alternative medicine use from May to July 2020. In the nine communities’ traditional healers were also interviewed on the type of herbal preparations used for COVID-19, mode of preparation and also on the signs and symptoms of COVID-19.
Study population
The population of the study included households from the nine communities. The study population included individual from the age of 21 years and above who were living for not less than six months in the community. The sampling units were households, while the study units were adult individual available in the household during the interview. The study population also included traditional healers residing in the communities.
Sample size determination
The Cochran formula was used to determine the minimum sample size required in this study. It allows for calculation of the best possible size with preferred precision and confidence level.
Sample size was calculated based on the prevalence of TCAM use following assumptions: p=50% (prevalence of TM use).
n=(z)2αp(1-p)d/i2
Where n=sample size; Za=constant; Confidence interval, 95%=1.96 at a=0.05; d=2.8 correction factor; i=Precision of the event of interest; degree of accuracy=0.05; p (population prevalence)=50%.
The prevalence of TCAM use in the Fako Division is unknown, therefore maximum heterogeneity was assumed (ie, a 50/50 split in users and nonusers) with p=0.5.
n=(1.96)2 α0.5(1-0.5)2.8/0.052
1078 participants
Considering a 2% non-response rate, a total of 1100 respondents were included in this study. Probability proportionate to size was used to determine the number of respondents that were recruited from each health district.
Sampling procedure
Systematic random sampling technique was used to select households in the nine communities. The first household per community was selected from the list of initial n households by balloting method. Then every nth household was selected and an adult in the household was interviewed. In the presence of more than one adult, balloting was done to choose one adult who was interviewed. Traditional healers were purposively selected to take part in the interview sessions from the study communities to assess herbal remedies used for COVID-19, mode of preparations well as the signs and symptoms (Table 1).
| District | ||
|---|---|---|
| Buea | 1,73,526 | 360 |
| Tiko | 1,54,690 | 320 |
| Limbe | 202, 831 | 420 |
| Total | 5,31,047 | 1100 |
Table 1. Sample size per health district based on probability proportionate to size.
The sample size per community, n/community=(Adult population of community/Total adult population of the 3 communities per district) × n (sample size per district) (Table 2).
| Study site | Total adult population | Number of participants per site (Proportionate sample) |
|---|---|---|
| Buea Town | 15,272 | 138 (38.3%) |
| Muea | 13,161 | 119 (33.3%) |
| Mile 16 | 11,321 | 103 (29.0%) |
| Total | 39,754 | 360 (100%) |
| Water Tank | 2,338 | 136 (42.4%) |
| Likumba | 2,743 | 159 (49.7%) |
| Small Ekange | 428 | 25 (8.0%) |
| Total | 5509 | 320 (100) |
| Mile 4 | 25,859 | 360 (85.7%) |
| Isokolo | 812 | 12 (3.0%) |
| Down beach | 3,469 | 48 (11.5%) |
| Total | 30,140 | 420 (100) |
Table 2. Sample size per study site based on probability proportionate to size among community participants.
Data collection procedures
Data was collected by trained data collectors using pre-tested semistructured questionnaires through face-to face interview. Structured closed and open ended questionnaire was adapted from standardized questionnaires such as the I-CAM (International questionnaire for CAM use) [13] and published articles in peer-reviewed journals. The questionnaire was divided into three sections: first section dealt with respondent’s information on the socio-demographic characteristics, the second section dealt with the use of TCAM in the past 12 months and for various ailments while the third section captured information on the community use of TCAM against COVID-19 and other ailments. Out of the 1119 copies of the questionnaire distributed, 1100 were returned in the community-based survey, giving a response rate of 98%. Interview guides were designed to capture information of the types of herbal preparation used by traditional healers for COVID-19 patients as well as the signs and symptoms for COVID-19.
Data quality control
Trained data collectors (postgraduate and undergraduate students) were used for the data collection process. The training involved a systematic and comprehensive explanation of the research process through extensive discussions. Included in these were questions and answers and demonstrations. The training also enabled the data collectors to acquaint themselves with field operations techniques. Pre-testing was done to validate consistency of the questions and data collection tool.
Study variables
The outcome variables of the study were prevalence of TCAM use and types of herbal remedies used for COVID-19 in the study area. The explanatory variables were age, location, monthly family income, educational status, religion, and ethnicity.
Data management and analysis
Questionnaires from the field were cross checked each time they were brought for unfilled and unanswered questions. Coding was also checked to ensure the use of correct codes by the principal investigator. Data was entered into excel, cleaned, and analyzed using SPSS Version 25 (Statistical Package for the Social Sciences) for Windows. The results were presented using simple frequencies with percentages in appropriate tables to display the descriptive part of the result. Multivariate logistic regression was used to determine the predictors associated with TCAM use. Atlas ti 7.5 (Scientific Software Development GmbH, Berlin) was used to code and analyze types of herbal preparations used for COVID-19 as well as the signs and symptoms. All statistical tests were performed using two-sided tests at the 0.05 level of significance.
Sociodemographic characteristics of respondents
A total of 1100 respondents, with a response rate of 98.3%, were studied. Table 3 describes their sociodemographic characteristics. Of the 1100 participants sampled, 420 (38.2%) (95% CI: 34.9-42.7) were drawn from Limbe, 320 (29.1%) (95% CI: 25.4-33.9) from Tiko and 360 (32.7%) (95% CI: 26.6-36.9) from Buea Health Districts following the principle of probability proportionate to size. Half (50.3%) (95% CI: 47.3-53.3) of the community members sampled were males. The mean age of the community members was 35.2 (SD=5.2) years and ranged from 21-78 years. Majority of the community members were either married or cohabiting 517(51.3%) (95% CI: 48.2-54.4), were self-employed 391(35.7) (95% CI: 31.8-40.0), had attained secondary school 572(53.7%) (95% CI: 50.7-56.6) and were Christians 1033(97.4%) (95% CI: 96.2-98.1). Majority 785(81.0%) (95% CI: 78.4-83.4) of the community members had an average monthly income less than 185 USD. Natives (Bakwerians) constituted only 202(18.5%) (95% CI: 16.3-20.4) of the sample. The mean number of people residing in a household was 5.67 (SD=1.2) and most 489 (44.7%) (95% CI: 41.8-47.7) of the households had between 4-6 members. Majority 786(76.0%) (95% CI: 73.3-78.5) of the community members resided in rural areas.
| Variables | Frequency no (%) | 95% CI |
|---|---|---|
| Age (years) | ||
| 21-30 | 286 (26.2) | 23.7-28.9 |
| 31-40 | 363 (33.2) | 30.5-36.1 |
| ≥ 41 | 443 (40.6) | 37.7-43.5 |
| Total | 1092 (100) | |
| Gender | ||
| Male | 538 (50.3) | 47.3-53.3 |
| Female | 532 (49.7) | 46.7-52.7 |
| Total | 1070 (100) | |
| Marital status | ||
| Single | 438 (43.4) | 40.4-46.6 |
| Married | 517 (51.3) | 48.2-54.4 |
| Widow/Divorced | 53 (5.3) | 4.0-6.8 |
| Total | 1008 (100) | |
| Occupation | ||
| Civil servant | 151 (13.8) | 11.9-15.9 |
| Private sector employee | 32 (2.9) | 2.1-4.1 |
| Self-employed | 391 (35.7) | 31.8-40.0 |
| Student | 392 (35.8) | 33.0-38.9 |
| Unemployed | 129 (11.9) | 8.7-15.3 |
| Total | 1095 (100) | |
| Religion | ||
| Christian | 1033 (97.4) | 96.2-98.1 |
| Muslim | 17 (1.6) | 1.0-2.5 |
| Traditionalist | 11 (1.0) | 0.6-1.8 |
| Total | 1061 (100) | |
| Education | ||
| No formal education | 35 (3.2) | 2.4-4.5 |
| Primary | 280 (26.3) | 23.7-28.9 |
| Secondary | 572 (53.7) | 50.7-56.6 |
| Tertiary | 179 (16.8) | 14.7-19.5 |
| Total | 1066 (100) | |
| Ethnicity | ||
| Native (Bakwerian) | 202 (18.5) | 16.3-20.4 |
| Others | 893 (81.5) | 79.2-83.5 |
| Total | 1095 (100) | |
| Monthly income (USD) | ||
| <185 | 785 (81.0) | 78.4-83.4 |
| 185-370 | 160 (16.5) | 14.3-18.9 |
| >370 | 24 (2.5) | 1.7-3.7 |
| Total | 969 (100) | |
| Household size (persons) | ||
| 1-3 | 348 (31.9) | 29.1-34.7 |
| 4-6 | 489 (44.7) | 41.8-47.7 |
| >6 | 256 (23.4) | 21.0-26.0 |
| Total | 1093 (100) | |
| Health district | ||
| Buea | 360 (32.7) | 26.6-36.9 |
| Tiko | 320 (29.1) | 25.4-33.9 |
| Limbe | 420 (38.2) | 34.9-42.7 |
| Total | 1100 (100) | |
| Environmental setting | ||
| Rural | 786 (76.0) | 73.3-78.5 |
| Urban | 99 (9.6) | 7.9-11.4 |
| Semi-urban | 149 (14.4) | 12.4-16.7 |
| Total | 1034 (100) |
USD: United States Dollars.
Table 3. Sociodemographic characteristics of participants.
Prevalence of TCAM utilization by community members in the Fako division
Of the 1100 community respondents sampled, 754 (68.5%) (95%CI: 66.3-71.5) had used TCAM in the last 12 months, 95%CI: 66.3-71.5. A majority of the participants from the Tiko Health District 415(72.2%) (95% CI: 70.6-73.6) use TCAM therapy followed by Buea Health District 328(69.9%) (95% CI: 72.6-72.6) and lastly by the Limbe Health District 284 (63.9%) (95% CI: 62.0-66.7) (Figure 1).
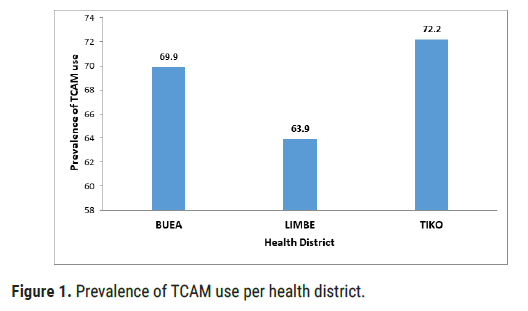
Figure 1: Prevalence of TCAM use per health district.
Category of persons using TCAM products and practitioners
Regarding the proportion of community members using TCAM, 42.8% (95% CI: 39.9-45.7) were adults, 23.8% (95% CI: 21.3-26.3) were elders, 18.6% (95% CI: 16.6-20.9) were pregnant women and 14.8% (95% CI: 12.7- 16.9) were children (Figure 2).
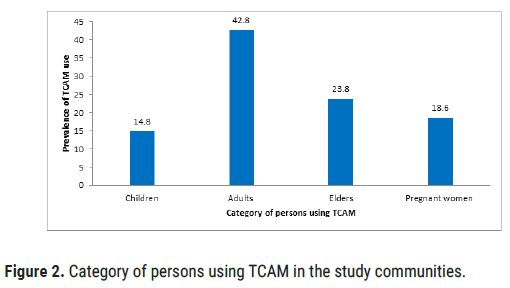
Figure 2: Category of persons using TCAM in the study communities.
Of the 754 community members using TCAM, 463 (61.4%) (95% CI: 58.5-64.3) used TCAM products (self-care and over-the-counter use), 141 (18.7%) (95% CI: 16.4-21.0) visited a TCAM practitioner and 150 (20.0%) (95% CI: 17.6-22.4) used both TCAM products and practitioner services in the past 12 months (Figure 3).
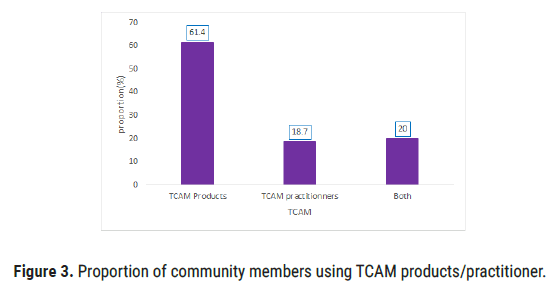
Figure 3: Proportion of community members using TCAM products/practitioner.
Based on the type of TCAM practitioner visited by the community members, 79.7% (95% CI: 77.3-82.1) visited herbalists, 14.9% (95% CI: 12.8-17.0) visited traditional bone setters, 3.4% (95% CI: 2.3-4.5) visited diviners, 1.3% (95% CI: 0.6-1.9) visited traditional birth attendants and 0.7% (95% CI: 0.2-1.2) visited massage therapists (Figure 4).
Based on the type of diseases for which community members visited TCAM practitioners, 44.6% (95% CI: 41.7-47.5) consulted because of acute diseases (disease <3 months), 43.4% (95% CI: 40.5-46.3) visited traditional healers for chronic diseases (disease >3 months) and 12.0% (95% CI: 10.1-13.9) for health promotion and disease prevention (Figure 5).
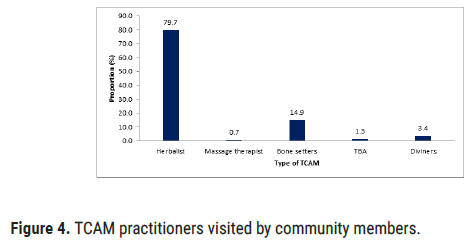
Figure 4: TCAM practitioners visited by community members.
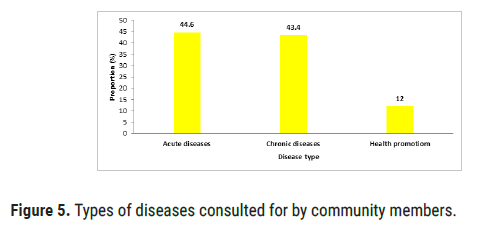
Figure 5: Types of diseases consulted for by community members.
Use of TCAM to prevent COVID-19
The proportion of community members reported they used herbal medicine to prevent COVID-19 was 24.4% (95%CI: 20.6-29.1). Of the 91 community respondents who used TCAM therapy, 22 (24.6%) (95%CI: 22.1-27.1) used garlics, 20 (22.5%) (95%CI: 20.0-24.9) used clove, 18 (20.1%) (95%CI: 17.7-22.5) used fever grass tea and 14 (15.4%) (95%CI: 17.5-17.5) used lemon tea (Figure 6).
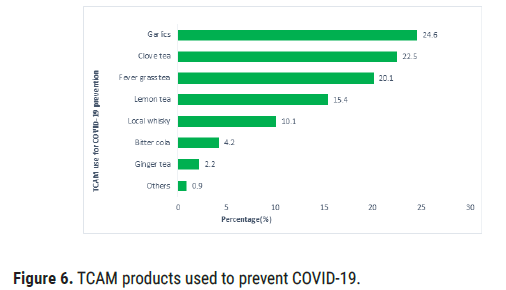
Figure 6: TCAM products used to prevent COVID-19.
Boiling was the most common methods of preparing herbal medicine for the treatment of various ailments (Table 4). Most of the herbal medicines required a mixture of many plants (concoction). The treatment duration ranged from 1 day to 7 days and the dosage was in glasses or cups (ranging from 1 glass to 3 glasses daily). The plants used were mostly from the gardens, herbalist, market, and environment or forest.
| Disease/ailments treated | Plant species use | Common name | Part of the plant use | Dosage form used | Route of administration | Method of preparation | Duration of treatment | Frequency | Source of plants |
|---|---|---|---|---|---|---|---|---|---|
| COVID-19, lung infections/Cough, | Azadirachta indica | Dogoyaro (Neem) | Leaves | Fluid | Mouth | Boiling-water | 3days | Twice daily | Herbalist |
| Allium sativum | garlic | Roots | solid | Mouth | Mouth | 3days | Twice daily | Market | |
| Zingiber officinale | Ginger | Roots | Solid | Mouth | Chewing | 2 days | Once daily | Environment | |
| Artemisia annua | Quinine stick | Entire plant | Fever | Boiling-others | Mouth | 3days | Twice daily | Garden | |
| Carica papaya | Pawpaw | Leaf | Fluid | Mouth | Boiling-others | 7 days | Twice daily | Environment | |
| Stomach/GIT disorders | Barbados aloe | Aloe vera | Leaf | Fluid | Mouth | Alone | 1day | Twice daily | Garden |
| Calpurnia aurea | - | Leaf | Fluid | Mouth | Alone | 3days | Twice daily | Forest | |
| Garcinia kola | Bitter cola | Seed | Solid | Mouth | Alone | 1day | Once daily | Market | |
| Senna alata | Eczema leaves | Leaf | Fluid | Mouth | Boil+moringa (seed) | 2weks | Thrice daily | Garden | |
| Spilantes filicaulis | Eye for fowl | Leaf | Solid | Mouth | Chewing | 3 days | Once daily | Garden | |
| Ocimum basilicum L | Masepo (Bakweri) | Leaf | Solid | Mouth | Chewing | 2 days | Once daily | Environment | |
| Fever (Febrile illnesses) | Bidens Pilosa | Black jack | Leaf | Fluid | Mouth | Boiling-water | 3 days | Twice daily | Environment |
| Moringa oleifera | Moringa | Leaf | Fluid | Mouth | Boiling-water | 3 days | Twice daily | Herbalist | |
| Cinchona officinalis | Quinine stick | Bark | Fluid | Mouth | Boiling-others | 4 days | Twice daily | Market | |
| Cymbopogon citratus | Fever grass | Leaf | Fluid | Mouth | Boiling-others | 3 days | Twice daily | Garden | |
| Psidium guajava | Guava | Leaf | Solid | Mouth | Chewing | 1 day | Thrice daily | Environment | |
| Helianthus annuus L | Sun flower | Leaf | Fluid | Mouth | Boiling-others | 7 days | Twice daily | Environment | |
| Carica papaya | Pawpaw | Leaf | Fluid | Mouth | Boiling-others | 7 days | Twice daily | Environment |
Table 4. Plants used by community members based on the diseases treated as derived from this study.
Use of herbal medicines by traditional healers to treat COVID-19
The most common signs and symptoms of COVID-19 reported by traditional healers was cough, catarrh, fever and joint pain. Boiling (concoction) was the most common methods of preparing herbal medicine for their patients. Parts of plants used ranged from leaves, roots, and seeds to whole plants (Table 5).
| Plant sp | Common name | Part of plant used | Symptoms of patient | Mode of preparation |
|---|---|---|---|---|
| Allium cepa | Onion | Dried leaves | Cough, Catarrh | Boiling |
| Aloe barbadensis | Aloe vera | Leaves | Cough, Fever | Boiling |
| Anthocleista djalonensis | Unbrella leaf | Bark | Cough, Fever | Boiling-others |
| Artemisia annua | Quinine stick | Entire plant | Fever | Boiling-others |
| Azadirachta indica | Leaves, stem and bark | Cough, Fever, joint pain | Boiling-others | |
| Cola nitida | Red cola | Leaves, seeds | Headache, Fever, Myalgia | Burn macerate+palm oil |
| Curcuma longa | Tumeric | Roots | Cough, Fever, body weakness | Boiling |
| Cymbopogon citratus, Fever grass | Leaves | Joint pain, fatigue, headache | Boiling | |
| Eucalyptus globulus | Eucalyptus | Leaves | Catarrh/Runny nose | Boiling |
| Eugenia caryophyllata | Clove | Seeds | Cough, Catarrh, headache | Boiling |
| Psidium guajava | Guava leaves | Leaves | Cough, fever, headache, sore throat | Boiling |
| Jatropha curcas | Big nuts plant | Leaves and fruit (nuts) | sore throat, cough | Boiling |
| Mangifera indica | Mango | Bark, leaves | Cough, Fever, Catarrh | Boiling |
| Melissa ofcinalis | Lemon balm | Leaves | Catarrh, Cough, Fever | Boiling |
| Moringa Oleifera | Moringa | Leaves and seeds | Cough, Catarrh | Boiling |
| Panax ginseng | Ginseng | Roots | Cough, Fever | Boiling |
| Paw paw leaves | Leaves | cough, fever | Boiling-others | |
| Pennisetumpurpureum Shum | King grass | Entire plant | Joint pain, fatigue | Boiling-others |
| Pimpinella anisum | Aniseed | Fruit | Cough | Boiling |
| Salvia officinalis | Sage | Leaves | Sore throat, cough | Boiling |
| Senna alata | Ezema leaf | Leaves | Cough fever, joint pain | Boiling-others |
| Thymus vulgaris | Garden thyme | Leaves | Cough, Catarrh | Boiling |
Table 5. Common plants used by traditional healers for the treatment of COVID-19.
Predictors of TCAM use in the communities
Multiple logistic regression model showed that age more than 41 years old had 2.23 (95% CI: 1.09-4.91) times the odds of using TCAM than people between 21-30 years. A farmer had 3.05 (95% CI: 1.99-5.34) times the odds of using TCAM than people from other occupations. Haven attained tertiary education 0.33 (95% CI: 0.16-0.88) were less likely associated with TCAM use compared to those with no formal education. Community members having between 100,000-200,000 FCFA as monthly income had 2.06 (95% CI: 1.33-4.55) times the odds of using TCAM than those with income levels below 100,000 Fcfa. Participants who resided in a rural setting had 2.30 (95% CI: 1.04-3.98) times the odds of using TCAM than those residing in an urban setting, being knowledgeable on TCAM had 3.10 (95% CI: 1.54-6.45) times the odds of using TCAM than not being knowledgeable on TCAM and having a positive attitude towards TCAM had 3.47 (95% CI: 1.94-6.45) times the odds of using TCAM than those with a negative attitude towards TCAM (Table 6).
| Variable | Use of TCAM | ||||
|---|---|---|---|---|---|
| TCAM use N (%) |
TCAM non-use N (%) |
AOR | (95% CI) | p-value | |
| Age (years) | |||||
| 21-30 | 177 (62.1) | 108 (37.9) | 1 | ||
| 31-40 | 239 (65.8) | 124 (34.2) | 1.11 | 0.81-3.68 | 0.138 |
| ≥ 41 | 336 (75.8) | 107 (24.2) | 2.23 | 1.09-4.91 | 0.018* |
| Total | 752 | 339 | |||
| Gender | |||||
| Male | 385 (71.6) | 153 (28.4) | 1 | ||
| Female | 354 (66.7) | 177 (33.3) | 0.71 | 0.45-2.15 | 0.113 |
| Total | 739 | 330 | |||
| Marital status | |||||
| Single | 287 (65.7) | 150 (34.3) | 1 | ||
| Married/cohabiting | 364 (70.4) | 153 (29.6) | 1.09 | 0.84-1.42 | 0.512 |
| Widow/divorced | 43 (81.1) | 10 (18.9) | 1.13 | 0.15-1.23 | 0.124 |
| Total | 694 | 313 | |||
| Employment status | |||||
| Employed | 395 (68.8) | 179 (31.2) | 1 | ||
| Unemployed | 359 (69.0) | 161 (31.0) | 1.01 | 0.80-3.09 | 0.534 |
| Total | 754 | 340 | |||
| Occupation | |||||
| Others | 700 (66.9) | 346 (33.1) | 1 | ||
| Farming | 54 (87.1) | 8 (12.9) | 3.04 | 1.99-5.34 | 0.002* |
| Total | 754 | 354 | |||
| Education | |||||
| None | 26 (74.3) | 9 (25.7) | 1 | ||
| Primary | 197 (70.4) | 83 (29.6) | 0.85 | 0.74-4.23 | 0.173 |
| Secondary | 405 (70.9) | 166 (29.1) | 0.95 | 0.26-4.15 | 0.236 |
| Tertiary | 105 (58.7) | 74 (41.3) | 0.33 | 0.16-0.88 | <0.001* |
| Total | 733 | 332 | |||
| Household size (persons) | |||||
| 1-3 | 228 (65.5) | 120 (34.5) | 1 | ||
| 4-6 | 336 (68.7) | 153 (31.3) | 0.81 | 0.65-1.15 | 0.243 |
| >6 | 188 (73.7) | 67 (26.3) | 1.01 | 0.87-3.21 | 0.255 |
| Total | 752 | 340 | |||
| Religion | |||||
| Christians | 717 (69.5) | 315 (30.5) | 1 | ||
| Muslim | 9 (52.9) | 8 (47.1) | 0.66 | 0.45-1.07 | 0.163 |
| Traditionalist | 5 (45.5) | 6 (54.5) | 0.78 | 0.54-2.35 | 0.235 |
| Total | 731 | 329 | |||
| Monthly income (USD) | |||||
| <185 | 527 (67.2) | 257 (32.8) | 1 | ||
| 185-370 | 127 (79.4) | 33 (20.6) | 2.06 | 1.33-4.55 | 0.004 |
| >370 | 10 (41.7) | 14 (58.3) | 0.41 | 0.23-0.98 | 0.012* |
| Total | 664 | 304 | |||
| Ethnicity | |||||
| Native (Bakwerian) | 140 (69.3) | 62 (30.7) | 1 | ||
| Others | 614 (68.8) | 278 (31.2) | 0.87 | 0.34-2.45 | 0.97 |
| Total | 754 | 340 | |||
| Environmental setting | |||||
| Urban | 558 (71.1) | 227 (28.9) | 1 | ||
| Semi-urban | 69 (69.7) | 30 (30.3) | 1.12 | 0.541 | |
| Rural | 86 (57.7) | 63 (42.3) | 2.3 | 0.89-2.35 | 0.022* |
| Total | 713 | 320 | 1.04-3.98 | ||
| Knowledge on TCAM | |||||
| Incorrect | 212 (64.4) | 117 (35.6) | 1 | ||
| Correct | 542 (70.3) | 229 (29.7) | 3.1 | 0.010* | |
| Total | 754 | 346 | 1.54-6.45 | ||
| Attitude towards TCAM | |||||
| Negative | 404 (66.0) | 208 (34.0) | 1 | ||
| Positive | 350 (71.7) | 138 (28.3) | 3.47 | 0.010* | |
| Total | 754 | 346 | 1.94-6.45 | ||
USD: United States Dollar.
Table 6. Determinants of TCAM use in the communities.
Prevalence and pattern of TCAM use in the study communities
This study revealed some interesting findings, some of which tally with literature and some that do not tally with prevailing trends of Traditional, Complementary and Alternative Medicine (TCAM) use. This study shows the prevalence of TCAM therapy use to be 68.5% which is lower than the 74.22% reported in Ethiopia, 77.5% reported in Nigeria [14] and also less than the 80% reported by the WHO. It was however greater than the prevalence of 58.2% obtained in a systematic survey for Sub Saharan Africa [6], and greater than the 60.0% TCAM use among respondents in Zimbabwe [15] and the 592 (55.5%) reported in Malaysia [16]. Differences in prevalence may be due to differences in study sites and in the sample sizes, as most studies in the systematic survey for SSA had sample sizes less than 500. The prevalence of TCAM use in Cameroon was much higher than that reported elsewhere in the industrialized world, ranging between about 29% in the USA to about 49% in Australia [17,18].
Based on the use of TCAM therapy by health District, Tiko (72.2%) and Buea (69.9%) Health districts recorded the highest users of TCAM therapy as compared to Limbe (63.9%) and this difference was statistically significant(X=5.632, p=0.056). This might be due to differences in location with the availability and accessibility to natural plants, coupled with mount Fako in Buea which is rich in diverse plant flora compared to Limbe. The majority of TCAM users were adults (42.8%), Elders (23.8%) and pregnant women (18.6%) while children (14.8%) were the least TCAM users. These population category was slightly different from that in Ethiopia where by complementary and alternative medicine was most commonly given to the elderly (32.62%), adults (24.11%), followed by children (17.02%) and pregnant women (2.13%) [19]. The prevalence of herbal medicine use among pregnant women was 18.6% which was less than that obtained in Nigeria 36.8% but greater than the 2.13% obtained in Ethiopia [20,21]. This can be due to the differences in the spatial distribution of the sample population. TCAM is highly use among the young adults despite their level of education and access to orthodox health services, which show that the knowledge and usage of TCAM is evergreen regardless of the ancient age of TCAM. Among the users of TCAM therapy, 61.4% use TCAM products while 18.7% visited TCAM practitioners only, while 20.0% use both. Studies conducted in Africa shows the prevalence of TCAM product use in the general population ranging from 4.6% (urban settlement in Ethiopia) to 94% (semi urban settlements in Nigeria and Ethiopia) with an estimated average of 58.2% [22-27]. Some studies reported on TCAM practitioner utilization (1.2%-67% (mean, 28.8%) [28-32]. A lower prevalence (1.2%- 44.1% (average, 12.6%) of TCAM practitioner services use was observed in studies with large sample sizes compared with other studies with smaller samples (37.5%-67% (mean, 53.0%) [32-37]. This was in line with our study with a large sample size of 1100 participants in the general population recording an 18.7% of TCAM practitioner use compared with smaller size sample sizes. This prevalence of TCAM practitioner use may be higher in disease specific subpopulations compared to the general population. Peltzer, et al. obtained prevalence of TCAM provider use, in Australia 34.7%, in Europe ranging from under 10% in Bulgaria, Poland and Slovenia to 35.4% in France, in Asia from 16.7% in Russia to over 50% in China mainland, the Philippines and Republic of Korea, and over 20% in the USA, Chile and South Africa [5]. The majority of the community members mostly use the services of herbalists, bone setters, followed by diviners. Similar findings were obtained in the Northwest Region of Cameroon where mostly the services of herbalists, traditional bone setters, diviners and traditional birth attendants where sorted for by the general population [38]. Our findings were similar to that in Tanzania where diviners, herbalists, traditional birth attendants, and bone setters were mostly visited by the general population [39]. Close to half of the population use TCAM for acute conditions (44.6%) or for chronic (43.6%) conditions while a small proportion use TCAM to maintain wellbeing. Our findings were not congruent with that obtained by Peltzer, et al. in which 53.7% of the participants used TCAM for treating a chronic or longterm health condition, 40.0% used TCAM in order to improve well-being and 6.3% for treating an acute illness [40]. According to Bannerman RH et al. complementary and alternative medicine is used by the people for the management of chronic conditions that are costly to society, such as chronic pain and arthritis, and more life-threatening diseases such as heart disease and cancer, which gives strength to the TCAM than orthodox, thus a need for integration to overcome the weaknesses of each [41].
Community use of TCAM to prevent COVID-19
Allium sativium (garlic), Azadirachta indica, Zingiber oficinale, Artemisia annua, Carica papaya were mostly used in combination with other plants to prevent COVID-19 in the communities. Our findings were similar to that obtained in previous studies i.e., in Madagascar a combination of artemisia, neem leaves, paw leaves, garlic, ginger, lime and oranges has been adopted as a notable anti-COVID agent [42]. These herbs are boiled together for 30 min and steam-inhaled. Expectedly the steam inhalation clears the lungs of the virus [42]. Our findings were also in line with that obtained in Nigeria in which phenolic compounds and antioxidant properties of these herbal remedies are known to contribute to their therapeutic effects [43]. Consumption of these Nigerian herbal remedies increase the anti-oxidant molecules and enzymes in the body and protect the cells and its membrane from being damaged by the toxic substances [43,44]. Phenolic moieties boost the body's immunity and defense against the threatening virus [45]. Scientists from the academia and Research Institutes have also supported the use of these herbal remedies as anti-COVID agents.
Herbal preparations used by traditional healers for COVID-19
This study brings out a number of herbal remedies used by traditional healers for COVID-19 which was congruent with that obtained by Fongnzossie, et al. [46] who reported the use of herbal remedies including Azadirachta indica, Zingiber oficinale, Artemisia annua, Carica papaya for the treatment of COVID-19 with symptoms such as sore throat, cough, catarrh, fever and jointpains. Azadiracta indica (neem) is one of the most used plants in the treatment of malaria in many parts of Africa and Asia where malaria is endemic. Roger, et al. provides proof that the neem plant can provide anti-viral effects for COVID-19 [47]. Similar plants species were reported as potential agents for COVID-19 in Ethiopia [48]. These included Lepidium sativum, Azadirachta indica, Osyris quadripartite and Allium sativum [48-51]. Citrus aurantium L., Citrus limon (L.), Capsicum annuum L., Eucalyptus globulus, Osyris quadripartite, Amaranthus hybridus Linn were also cited as effective against COVID-19 [51].
Determinants of TCAM use in the general population
Age above 41 years, farming as occupation, having attained tertiary education, having a monthly income above 185 USD, residing in a rural setting, being knowledgeable on TCAM and having a positive attitude towards TCAM were strongly associated with the use of TCAM. However, age group was different compared with other study as ages between 18- 28 and 29-38 years were associated with the use of TCAM in Ethiopia [52]. Similar findings were obtained in the Bui-Division of Cameroon where most patients reported visiting the traditional healers because of the low cost (69%) and low level of income [53].
Our findings were also congruent with Karl, et al. in which middle age, being a female, lower educational status, not having a religious affiliation, larger household size, not having a health insurance, could not pay for medical treatment when needed it were associated with TCAM provider use [40]. Also the authors showed that having a chronic condition or disability, and having positive attitudes towards TCAM (TCAM being better than mainstream medicine and TCAM does not promise more than it can deliver) significantly increased the odds of TCAM provider use. However, our findings were different from that obtained from Cambodia whereby being a female (AOR=1.42, 95% CI=1.12-2.67), haven completed less schooling (AOR=0.66, 95% CI=0.45-0.96), unemployed or homemakers (AOR=0.23, 95% CI=0.13-0.52) and have a gastrointestinal illness (AOR=0.49, 95% CI=0.39-0.62) were associated with TCAM use [54]. Findings were similar to that obtained in Ethiopia whereby age (P=0.02), especially age group between 18 and 28 and 29 and 38 ((P=0.02 and 0.004, resp.), educational status was also significantly associated with TCAM use (P=0.00). Moreover, occupation (P=0.00) and effectiveness of TCAM (0.002) were found to be associated with TCAM use [52]. Our findings were however different from study in the general population in Ghana which shows that TCAM use was predicted by having low-income levels (Odds Ratio (OR) 2.883, Confidence Interval (CI) 1.142-7.277), being a trader (OR 2.321, CI 1.037-5.194), perceiving TCAM as effective (OR 4.430, CI 1.645-11.934) and safe (OR 2.730, CI 0.986-4.321), good affective behavior of traditional medical practitioner (TMP) (OR 2.943, CI 0.875-9.896) and having chronic ill-health (OR 3.821, CI 1.213-11.311) were associated with TCAM use [55]. Differences in the predictors of TCAM use may be due to difference in study population.
Prevalence of TCAM use was measured within a standard pattern of TCAM use within the past 12 months. As a limitation to this study there is the possibility of recall bias and thus an under or over reporting of prevalence for TCAM use. Thus to overcome this, further questions were asked and a large sample size to overcome such limitations.
Our study found that TCAM are broadly used among community members in the Fako Division of Cameroon. More than half of the population having used TCAM in the last 12 months. The most commonly used TCAM was herbals. Allium sativum, Azadirachta indica, Zingiber oficinale, Artemisia annua were most commonly used TCAM for COVID-19. Occupation, level of education, monthly income, environmental setting, good knowledge and positive attitudes were associated with TCAM use.
Ethics approval and consent to participate
Ethical clearance was obtained from the Faculty of Health Sciences Institutional Review Board (FHSIRB) (Reference Number: 2018/952-03) of the University of Buea. Following the review and approval of the research proposal by FHSIRB, an administrative authorization was obtained from the Regional Delegation of Public Health, South West Region. Each study participant agreed to participate voluntarily. Participants were allowed to discontinue the interview when they needed. All participants of the study declared their willingness to participate and approved by their written and verbal consents. Participant’s information was kept confidential and codes were used on the questionnaire and interview guides.
Not applicable.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
This study was conducted independent of employment and the author declares no financial assistance was given nor any financial gain is promised as a result of publication. The authors declare that they have no competing interests.
ACW participated in the conception, designing, conducted the data collection, analysis and drafting of manuscript. NNT participated in the drafting, read and corrected the manuscript; ANJC participated in design, supervision, drafting of the manuscript and substantially revised the manuscript for academic content. NDS participated in the conception, oversaw the data collection process and analysis, supervised the work and substantially revised the manuscript for academic content. All authors read and approved the final copy of the manuscript.
The authors will like to express their sincere appreciation to the community respondents, the community leaders including some local chiefs that were visited as bottle necks and the Regional Delegation of Public Health for the South west Region who have contributed in making this study possible and successful.
Citation: Ayima CW, et al. Prevalence and Predictors of Traditional, Complementary/Alternative Medicine Use, and Types of Herbal Remedies used for COVID-19 in the South West Region of Cameroon. J Biol Today's World, 2021, 10(6), 001-004.
Received: 15-Sep-2021 Published: 06-Oct-2021
Copyright: © 2021 Ayima CW, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.