Case Report - (2022) Volume 3, Issue 5
This clinical report represents the prosthetic management of a severe dentofacial deformity with compromised periodontal status. On the basis of clinical, radiographic examination and mounted diagnostic casts treatment objectives were made which included aesthetics enhancement, socio-psychological support of the patient, restoration of form & function along with improvement in phonetics and comfort. The treatment sequence included extraction of upper incisors followed by alveoloplasty, thereafter an immediate removable partial denture was fabricated, this was followed by replacement of incisors by a metal-ceramic fixed partial denture.
Incisors protrusion • Alveoloplasty • Aesthetics • Fixed partial denture
The mouth is the focal point of many emotional conflicts and the f irst source of human contact with the world. A smile, when pleasing and attractive to observers, enriches not only the one who smiles, but those who view it [1]. It is an accepted fact that dentofacial aesthetics and psychological wellbeing is the dual maestro influencing everybody in day-to-day life. Visible dental characteristics that deviate greatly from the norm may stigmatize or impede career development and peer group acceptance, have a negative effect on self-concept, and encourage negative stereotypes [2]. Vertical Maxillary Excess (VME) compounded with severe localized periodontitis with extreme proclination of incisors with or without other dentofacial deformities in a middle-aged patient is a clinical challenge for the orthodontist as well as to maxillofacial surgeon in terms of predictable aesthetics and stability [3]. This clinical report documents the prosthetic rehabilitation of a 27-years-old woman, having VME with severely proclined incisors.
A 27-year-old female patient reported to the department of periodontics with the chief complaint of severely proclined maxillary incisors and was totally unsatisfied with her appearance and desired improved esthetics (Figure 1).

Figure 1: Pretreatment extraoral view.
Intraoral examination
The patient presented with bilaterally Angle's Class I molar relation with severely protruded maxillary incisors and a large overjet, Grade III mobility of maxillary anterior teeth, deep pockets, pathological migration, and spacing between maxillary anterior teeth. The mandibular anterior teeth presented with moderate to severe gingivitis. The occlusion was Group function bilaterally (Figure 2).
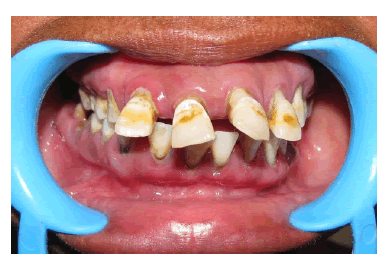
Figure 2: Pretreatment intraoral view.
Radiographic examination
Panoramic and IOPA radiographs revealed the trabecular bone pattern was generally normal with severe bone loss around maxillary anterior teeth. Root morphology of canines was favorable with a crown-to-root ratio of 1:2. Lateral cephalogram revealed anterior dentoalveolar protrusion of maxillary incisor region with Class-l molar relation (Figure 3).

Figure 3: Pretreatment lateral cepalalogram.
Treatment plan
Based on clinical and radiographic findings, articulated casts, and considering the patient’s views treatment plan was based on aesthetic enhancement, socio-psychological support to the patient, and restoration of function, phonetics, and comfort [4]. So, the prosthetic rehabilitation of the case was decided in two phases as follows:
Phase I:
1. Oral prophylaxis.
2. Mock-up of alveoloplasty on diagnostic casts.
3. Extraction of maxillary incisors and alveoloplasty.
4. Immediate removable partial denture.
Phase II:
1. Fixed Prosthodontic restorations using PFM (porcelain fused to metal) full veneer retainer replacing maxillary incisors.
After explaining treatment plan, including the risks and benefits of treatment, patient consent was taken.
Treatment sequence
Three sets of study casts were made for records and treatment planning. Face bow transfer was done and casts were mounted on Hanau articulator (WaterPik Technologies Inc USA). In the first phase of treatment, patient received oral prophylaxis. On diagnostic cast maxillary incisors were trimmed and a tentative alveoloplasty mock-up with labiolingual reduction of around 4 mm was done. A surgical template cum RPD (Removable Partial Denture) was fabricated on the mock-up cast for immediate insertion after alveoloplasty. The shade of the teeth was selected before extraction for future use. Maxillary incisors were extracted, alveoloplasty with labial reduction of 4 mm was done and surgical template cum-RPD was inserted immediately (Figures 4 and 5). The patient was instructed not to remove the denture till the next scheduled appointment 48 hours postoperatively. The patient was then instructed to wear the RPD for the next 4 weeks-6 weeks to allow complete healing of the site as well as to evaluate aesthetics, phonetics, and function with the prosthesis.
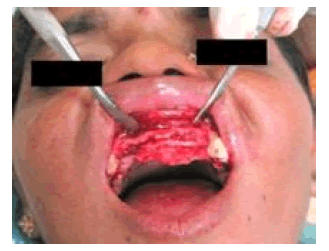
Figure 4: Extraction of incisors and alveoloplasty.

Figure 5: Immediate removable partial denture inserted.
The second phase of the treatment procedure was initiated after six weeks (Figure 6). Meanwhile the diagnostic wax-up was designed on the mounted cast to set up incisal guidance in harmony with esthetics, phonetics, and function and to create a template for the fabrication of provisional restoration [4].
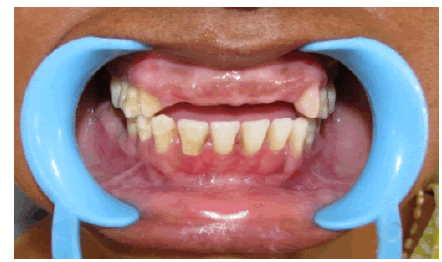
Figure 6: Six weeks after surgery and abutment tooth preparation.
Abutment teeth (13, 23) were prepared for metal-ceramic restorations with a sub-gingival finish line of radial-shoulder and chamfer design [5] (Figure 6). Definitive impression was made using vinyl polysiloxane impression material (Aquasil Putty and XLV, Dentsply, USA) and final casts were generated from type IV die stone (Ultrarock, Kalabhai Dental, India). Occlusal registration was made using Vinyl polysiloxane bite registration material.
Provisional restorations (Protemp, 3M, USA) were fabricated using an indirect technique and were evaluated intra-orally, adjusted for centriceccentric contacts. The patient was recalled after 4 weeks to re-evaluate the esthetic, phonetic, comfort, and function with provisional restorations. Metal ceramic FPD (Fixed partial Denture) was fabricated and tried in. Margins, proximal contacts, and occlusion were evaluated intra-orally, adjusted, and cemented with glass ionomer cement (Fuji I, GC America, lnc) (Figures 7-9).

Figure 7: Post-treatment intraoral view.

Figure 8: Post-treatment extra oral view.

Figure 9: Post-treatment lateral view.
Instructions to patient
Oral hygiene instructions were given, emphasizing cleaning the restoration margins using dental floss. The patient was seen at 2-weeks, 1-month, 3-months, and 6-months follow up and kept on every 6-month recall appointments.
This case illustrates the importance of proper diagnosis and treatment planning. At an early age, a team approach with the orthodontist, periodontist, and restorative dentist can produce better results but because of the age of the patient and compromised bone support to the affected dentition, the best way to achieve stable, functional, and aesthetic results, in this case, was the prosthetic approach. Through this approach, the patient had a dramatic dentofacial improvement. The patient has reported confidence in self-esteem and was pleased with her appearance
Citation: Kamboj, A. Prosthetic Correction for Aesthetic enhancement- A Case Report. J General Dentistry, 2022, 3(5), 001-003.
Received: 02-Jul-2022, Manuscript No. JGD-22-71274 ; Editor assigned: 04-Jul-2022, Pre QC No. JGD-22-71274 (PQ); Reviewed: 10-Jul-2022, QC No. JGD-22-71274 (Q); Revised: 12-Jul-2022, Manuscript No. JGD-22-71274 (R); Published: 20-Jul-2022, DOI: 10.35248/dentistry.3.5.01-03
Copyright: © 2022 Kamboj A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited