Research - (2022) Volume 14, Issue 9
Introduction: Chronic pain and mental health disorders are common in the general population, the prevalence of chronic pain ranges from 2% to 40%, and the prevalence of mental health disorders ranges from 17% to 29%. Chronic pain is associated with irritability, depression, anxiety, and sleep problems such as insomnia. However, the appearance of both has been described as a consequence of the characteristics of this pathology.
Aims: Determine the sociodemographic characteristics and the association between pain syndromes and mood disorders in individuals treated in primary care.
Materials and methods: A prospective cohort study was performed in a primary care medical center where patients with painful symptoms like reasons for consultation were taken for four months, to who scales such as DN4, VAS, Beck's criteria, DSM- V, and determined the sociodemographic characteristics of these individuals.
Results: A total of 132 patients were recruited who met the inclusion criteria, of which 81.81% (108) were women, 18.18% were men (24), the mean age in years for both sexes was 37.9, the mean Duration in hours of each painful episode is 14.35 hours, in terms of proportion the appearance of the disorders that we determined to evaluate obtaining: insomnia in 0.303, anxiety 0.265, depression 0.090, which coursed with anxiety or depression at the time with a type disorder mixed 0.053, patients who did not develop any of the diseases of interest in this study 0.185.
Discussion: The coexistence and overlap of mood disorders and insomnia in patients suffering from pain syndromes, which have little or no importance when assessing patients in primary health care centers, are underdiagnosed. However, broadening the clinic history, and correctly using diagnostic tools for mood disorders increases their diagnosis rate, ignoring the positive relationship that exists between these disorders.
Conclusions: Pain disorders trigger neuropsychiatric complications, depression, anxiety, and insomnia worsen episodes of pain. However, the correct diagnostic approach and the application of adequate management greatly reduce the complications of these types of disorders.
Chronic pain • Depression • Sleep disruption • Diagnostic
Pain syndromes currently represent a very important reason for consultation in medical settings, from primary practices to higher level hospital departments, often with the coexistence of mood disorders such as anxiety/depression, or sleep disorders such as insomnia, overlapping their symptoms, demonstrating the importance of understanding between these disorders, which in many cases are overlooked by physicians [1, 2]. Previous studies on chronic pain and its association with mental disorders have shown generally consistent findings, but they have some limitations, as they cannot establish the components as a whole from neurobiology [3-6].
Pain is a subjective experience influenced by different biopsychosocial factors, defined a s a m ultidimensional a nd subjective experience, the International Association for the Study of Pain defines p ain a s "an unpleasant subjective sensation and an emotional experience associated with actual or potential tissue damage", and is considered a debilitating disease when it becomes chronic [7, 8]. Chronic pain defined by the International Association for the Study of Pain and the International Classification of Diseases (ICD 11) is considered as pain that lasts more than 3 months or as persistent or intermittent pain for more than three months, leading to serious consequences. such as the impact on the patient's quality of life, including mood, sleep, and cognitive processes [9,10]. Anxiety is described as increased expectations and increased feelings of fear, worry, apprehension, and dread, while depression is described as feelings of sadness, grief, hopelessness, worthlessness, and pessimism [11,12]. The link between chronic pain and its affective components (i.e., depression and anxiety) has been known since the time of the ancient Greeks [13,14]. There is evidence of synchronicity between painful symptoms and symptoms of mood disorders; depression/anxiety, pain, and insomnia are positively correlated. Chronic pain and mental health disorders are common in the general population; the prevalence of chronic pain ranges from 2% to 40%, and the prevalence of mental health disorders ranges from 17% to 29% [15-17]. Chronic pain is associated with many other symptoms in about 1/3 of patients, including a combination of irritability, depression, anxiety, and sleep problems such as insomnia. It is also associated with cognitive dysfunctions, such as attention, learning, memory, and decision-making problems, as well as cardiovascular diseases [18,19].
The majority of people living with chronic pain, and overlapping symptoms of mood disorders, experience episodes of poor-quality sleep and it has been estimated that people with these factors are 18 times more likely to meet the criteria for a diagnosis clinician of insomnia [20- 22]. Although a bidirectional relationship between these symptoms and the coexistence of these conditions has been observed, it may presage common biological and, in some cases, psychological mechanisms. There is increasing evidence of pathophysiological, and neurophysiological similarity demonstrating that these conditions are associated with dysregulation of modulatory neurotransmitters along shared neuroanatomical pathways. Therefore, the decrease or dysregulation of the neurotransmitters involved can increase peripheral pain signals, which can contribute to the frequent presence of painful symptoms [23, 24].
This inferred direction of causality has important clinical implications; whether improvements in sleep and symptom presentation of mental disorders lead to reductions in pain, and how antidepressants that increase neurotransmitters involved in pain pathways reduce pain signals [25-27]. So sleep and mood disorders, as potentially modifiable factors, may be a viable target for interventions that can lead to significant improvements in treatments and outcomes that aim to reduce the intensity of chronic pain presentation if also associated mental disorders are treated [28-31]. On the other hand, it should be noted that as progress has been made in the study and understanding of the treatment of pain, a large number of epidemiological studies have described the association that may exist between this pathology and mood disorders. However, in the context of Colombia and Latin America, there are few studies carried out to date regarding this problem, which is why the generation of updated data according to our health environment is of great importance.
A prospective cohort study with retrospective analysis was proposed to determine the association between pain syndromes and mental disorders such as anxiety, depression, or insomnia from primary care, since these are the most frequently described in the current literature, so it was carried out in a primary health care center in the south of the city of Bogota-Colombia, where a population with low socioeconomic resources is characterized. For which the recruitment of patients attending the consultation was proposed and as inclusion criteria, a painful symptom was determined as a reason for consultation and that during the consultation they presented symptoms of anxious characteristics, negative depressive symptoms or that also manifested sleep compromise, A total of 464 patients attended by two doctors per month were taken during the interval from April to July of the year 2022, of which the reasons for consultation of interest were filtered, obtaining 132 individuals (28.45%) of the total number of patients attended, in who through the anamnesis were applied scales endorsed for the diagnosis of mental disorders in the spectrum of anxiety, depression or insomnia such as Beck criteria, DSM-V criteria, for these disorders and the DN4 test was applied and VAS (Visual Analog Pain Scale) for each type of pain, as they were diagnosed during the consultation, they were included in a database data. The locations and associated pain syndromes, the coexistence of comorbidities, and the time of evolution of painful symptoms and insomnia, depression, or anxiety were also described, in addition, the periods of duration of each painful episode and whether they worsened were also inquired recorded the history of pharmacological management for some of these syndromes.
After collecting the data, the analysis of these was carried out with the statistical program R version 4.1.3, evaluating the distribution by sex, age, and the prevalence of each pain syndrome in the sample taken. The data record was crossed with the simultaneous appearance of insomnia, anxiety, or depression, determining the cumulative incidence CI of the same, the statistical determination of the relative risk RR of anxious, depressive disorders, or insomnia associated with pain was also carried out, the mean was determined for the duration of the episodes of pain at the same as for the time of evolution of the same, however, in this item, it was not possible to determine the time of appearance of the disorders of interest with the pain syndromes given the moment in which the patients consulted it was difficult to determine exactly within the assessment the interval of appearance of symptoms of insomnia, anxiety or depression. Finally, the response to the proposed treatment was evaluated per the recommendations in the clinical practice guidelines and the recent publications in two months in this group for some of these disorders as adjuvant or treatment of some of these associated disorders after treatment. the query.
A total of 132 patients were recruited who met the inclusion criteria, of which 81.81% (108) correspond to women and 18.18% to men (24), the mean age in years for both sexes is 37.9, the mean duration in hours of each painful episode is 14.35 hours, the average evolution in months for the sample taken is 16.17, on the other hand, all manifestations of painful symptoms such as headaches, migraines, and even facial dysesthesias, finding that 35.6% (47) of the individuals presented with some of these manifestations. In the back pain group, patients with lumbar pain only or with pain at this level and at higher levels such as dorsal pain were included. or cervical, finding that 35.6% (47) of the patients also presented with this symptomatology, we made a separate group of joint pain for the different types of pain at the level of the shoulders, whether it was syndrome rotator cuff, shoulder abduction pain, tendinopathies or impingement in the group of muscle pain syndrome since we determined in this disorder a large percentage for the total sample of 11.36% (15), in the group of joint pain we included patients with knee pain, or arthralgia due to arthritis or osteoarthritis in different anatomical locations with a total of 6.81% (9) and in the group of others we included different subjects who had a variety of painful entities such as an individual who had chronic pain in the lower left limb after a fracture of the tibia and fibula who underwent surgical management presenting chronic pain and subsequent development of insomnia secondary to pain, also patients with epicondylitis or carpal tunnel syndrome for a total of 10.60% ( 14).
We calculated in terms of proportion the appearance of the disorders that we evaluated, obtaining: insomnia at 0.303, anxiety at 0.265, depression at 0.090, individuals who had anxiety or depression at the same time as a mixed-type disorder at 0.053, patients who had other previous mental pathologies such as bipolar affective disorder, schizoaffective disorder, schizophrenia or post-traumatic stress disorder showing 0.098 and finally the patients who did not develop any of the disorders of interest in this study 0.185 (Figure 1).
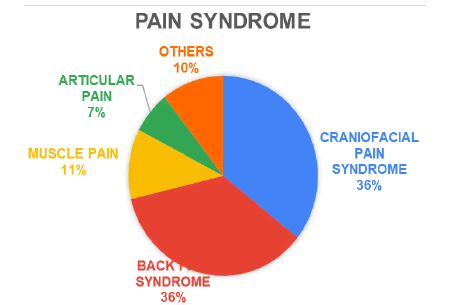
Figure 1: Distribution of pain syndromes.
The accumulated incidence was determined according to what was evidenced in the sample and since we did not know the total population that could be consulted in our medical center, 0.82 was obtained for the collected sample, according to this we also determined the calculation of the Relative Risk (RR) adjusted for the sample, which is 2.82 for the development of anxiety, depression or insomnia or mood disorders. Finally, after one month of treatment, we evaluated the improvement in pain levels according to the recommendations of the international guidelines for the management of insomnia, anxiety, or depression, including tricyclic antidepressants such as amitriptyline, serotonin reuptake inhibitors such as trazodone. or sertraline or double receptors of serotonin and norepinephrine such as paroxetine, however, given the initial objective of this study, we did not compare the results between these, but rather, whether they improved anxious, depressive or insomnia symptoms, with evidence of a reduction in headache. At least 4 points on the visual analog pain scale in 89% of the patients who simultaneously had these pathologies (Figure 2).
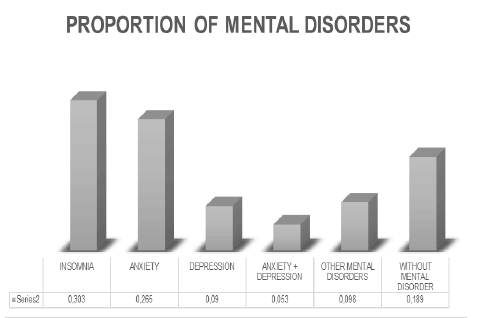
Figure 2: The proportion of mental and mood disorders associated with pain syndromes.
The appearance of mood state disorders in primary care consultation is usually underdiagnosed if it is evaluated as the main reason for patient consultation, however, as has been described in the literature to date, these figures increase when an extension is made in the anamnesis. The coexistence and overlap of mood disorders and insomnia in patients suffering from pain syndromes, which have little or no importance when assessing patients in primary health care centers, is demonstrated. being underdiagnosed as well as expanding the anamnesis, and correctly using diagnostic tools for the disorders of interest in this study, which the current literature describes, increases their diagnosis rate by ignoring the positive relationship that exists between these disorders, and ignoring a fundamental pillar in the comprehensive treatment for these patients, in which there is more scientific evidence every day [32-37].
Regarding the results, we obtained, we showed how women continue to be the most affected in the development of mental disorders in the course of pain syndromes, with the most affected anatomical areas being the spine and the head. represents an almost 3-fold risk of developing insomnia or anxiety, mainly which, if evaluated according to the descriptions of the anatomical and neurobiological pathways that these syndromes share, we could assert that it is a neuropsychiatric risk factor to have alterations in the pain spectrum; In comparison with what has been described in different studies in our context, the prevalence of depression has been described above or as frequently as anxiety, however, we obtained that in our environment anxiety and insomnia occur more frequently, which we consider represents the alterations that they present more prematurely in pain disorders, in this way we determine that the associated neuropsychiatric disorders present according to the time of evolution. We were also able to evidence anecdotally how subjects who do not receive correct initial management of a pain syndrome, such as the case of the individual who progressed with a tibia fracture, can first develop chronic pain and subsequent insomnia. Although it was not the objective of this study, we were able to show how, by applying the existing recommendations to date for pharmacological therapy, the spectrum of pain syndrome and neuropsychiatric disorders is reduced, and last but not least, we highlight how the application of the tools adequate even by non-specialized medical personnel represents better outcomes for these patients.
It is noteworthy within the results obtained that, although painful disorders trigger neuropsychiatric complications, depression, anxiety, and insomnia worsen episodes of pain. The application of adequate tools and the correct way of primary health care represents a considerable impact in the management of patients with painful disorders and simultaneously in the management of patients with mental disorders that are usually underdiagnosed in primary care and also develop capacities on the part of this personnel to assume the follow-up and management of these patients when access to medical specialties is limited or tortuous for the affected individuals. In addition to this, interdisciplinary management is recommended in conjunction with the mental health area, to guarantee adequate and timely treatment, and to avoid the development of mental disorders due to pain syndromes.
Citation: Rodriguez EM et al. Relationship Between Anxiety/Depression Mood Disorders and Insomnia in Patients with Pain Syndromes in Primary Health Care: A Cohort Study. 2022, 14 (09), 001-004
Received: 07-Sep-2022, Manuscript No. IJCRIMPH-22-74020; Editor assigned: 10-Sep-2022, Pre QC No. IJCRIMPH-22-74020; Reviewed: 15-Sep-2022, QC No. IJCRIMPH-22-74020; Revised: 19-Sep-2022, Manuscript No. IJCRIMPH-22-74020; Published: 30-Sep-2022, DOI: 10.35248/1840-4529.22.14.9.383
Copyright: ©2022 Rodriguez EM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.