Case Report - (2020) Volume 9, Issue 5
Malaria is the world's leading parasitic endemic, particularly in sub-Saharan Africa, where it is a real public health problem despite enormous efforts to combat it. It is accepted that in these WHO African regions, malaria is mainly caused by P. falciparum and rarely by other species. The cases of severe malaria encountered there are often caused by plasmodium falciparum. The authors report a case of severe malaria with plasmodium oval, in a young Senegalese patient who had spent two months in Guinea Conakry.
Severe malaria, plasmodium oval, Adult, Senegal.
Malaria is the world's leading parasitic endemic, particularly in sub-Saharan Africa, where it is a real public health problem despite enormous efforts to control it [1-3]. Recent epidemiological data indicate that it is still sub-Saharan Africa that bears the global malaria burden and it is accepted that in these WHO African regions, as well as in the majority of countries worldwide, malaria is due to P. falciparum, incidentally to P. oval and more rarely to P. malariae and vivax [1-5]. However, the cases of severe malaria encountered, especially in sub-Saharan Africa, are often due to plasmodium falciparum [2,3,6], and there is little statistical evidence of severe malaria in adults [7,8]. Less frequent cases of severe malaria due to other Plasmodium species have been reported worldwide, including Plasmodium Knowlesi [9], Plasmodium vivax [10-13], and a few reported cases involving plasmodium oval [6,14-16].
We report the case of a 26 year old Senegalese patient who presented a persistent infectious syndrome after returning from a trip to Guinea Conakry, in whom QBC and then blood smear revealed plasmodium oval. The evolution was favorable under artesunate injection.
OB is a patient of Senegalese nationality who spent two months in Guinea Conakry and returned to Senegal one week before the onset of his illness. He was seen on 29 December 2019 in a health facility in Dakar for headache associated with fever and abdominal pain, which led to the suspicion of typhoid fever or malaria. After a negative rapid diagnostic test (RDT), two thick drops were administered 48 hours apart, as well as a serological diagnosis of Widal and Felix. The results were in favor of a progressive minor salmonellosis, the thick drops being negative. The patient was thus treated on an outpatient basis with ciprofloxacin combined with paracetamol. He consulted again on 01/01/2020 in our structure in front of the absence of improvement of his symptomatology. The clinical manifestations were then dominated by malignant hyperthermia at 40.8°C, hyperalgesic headaches not relieved by analgesics, a feeling of vertigo.
A new RDT was performed but still negative. Laboratory results showed, the CRP elevated to 210 mg/l, thrombocytopenia (platelets=190,000) and normochromic macrocytic anemia with a hemoglobin level of 11.1 g/l.
He was hospitalized for better management and was treated with dual parenteral antibiotics (ceftriaxone, combined with gentamicin).
The course was marked by persistent fever, headache and prostration, followed by a disorder of consciousness with stage I coma. In front of these signs, we carried out another assessment including: a thin blood smear, a QBC, a blood culture, a feacal bacteriological examination, retroviral serology, HbsAg, a renal assessment and liver function tests. The QBC, and then thin blood smears test allowed the isolation of an oval plasmodium with an estimated parasite density of 1% parasitized red blood cells per field (Figures 1 and 2).
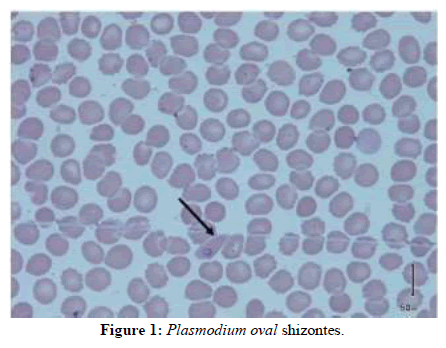
Figure 1: Plasmodium oval shizontes.
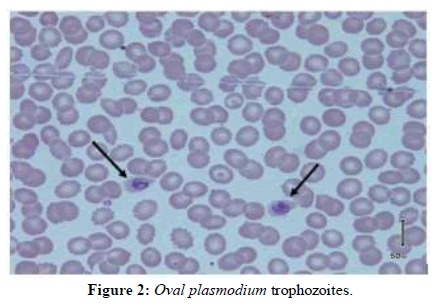
Figure 2: Oval plasmodium trophozoites.
HbsAg was positive, retroviral serology was negative and other investigations were unremarkable. Blood and faecal cultures were also negative.
Treatment with artesunate injection was then administered and resulted in a disappearing fever after 48 hours, regression of headache and rapid restoration of consciousness.
Despite the high prevalence of malaria in sub-Saharan Africa, there are very few studies of severe malaria in adults [7,8,17]. Our observation concerns a case of severe plasmodium oval malaria in an adult. The initial clinical picture on admission was dominated by fever and headache, followed by prostration and altered consciousness. Diallo et al. reported in their studies the same clinical manifestations at admission, but in the series of Rakotoarivelo RA disorders of consciousness were at the forefront [7,8,18].
From a paraclinical point of view, the thick drop and the thin blood smear have been the two most widely used parasitological diagnostic techniques [7,8,18].
Biological diagnosis by light microscopy remains the reference examination to confirm malaria cases [2-4]. However, light microscopy can be negative in the case of P. oval, hence the importance of complementing it with PCR or other available diagnostic tools. Diallo in a Senegalese study, and Rojo in Spain had to use PCR to identify P oval, despite the contribution of experts’ microcopist in the thick [14-20]. As in our observation, Eholié used QBC, in some cases where the EG was negative, to confirm the diagnosis [17]. plasmodium oval was found on a blood smear, associated with plasmodium falciparum in two cases of severe malaria reported in the cohort of Adnane while in the studies of Rakotoarivelo, Eholié and DIALLO, only plasmodium falciparum was found [7,8,17,18].
Ourpatientbenefitedfromtreatmentwithartesunateinjection, with a favourable evolution within 48 hours. Recommended by the WHO in the face of the emergence of strains of plasmodium resistant to traditional malaria treatments and adopted by certain countries in sub-Saharan Africa, artesunate injection is more than a simple alternative, an effective and easy-to-use antimalarial drug.
Malaria remains a major public health problem in many countries around the world and particularly in sub-Saharan Africa. Severe forms are often confined to plasmodium falciparum, but cases of severe malaria due to other species are reported, although underestimated. When there is any doubt about a feverish state with RDTs or even Thick film negative in malaria endemic areas, other diagnostic means, if available, should be used to limit the risk of complications due to malaria.
Received: 13-Apr-2020 Published: 05-May-2020
Copyright: �?�© 2020 Noubadoum A, et al. This is an open access paper distributed under the Creative Commons Attribution License. Journal of Biology and Today's World is published by Lexis Publisher.