Case Report - (2019) Volume 11, Issue 1
In the current era of medicine, more transplants are performed than ever before. Many kidney transplant recipients are elderly with numerous comorbidities. There has been a rise in trauma related injuries around the world. Hence it can be argued that we are more likely to see traumatic injuries in renal transplant recipients. Due to multiple medications, comorbidities and extra peritoneal location of the transplant kidney, the transplant graft is likely to get involved and its management would not be straightforward. There is a lack of consensus regarding the management of allograft following trauma in kidney transplant recipients. A general principle is life before the graft; however in situations where patient is stable and there is an isolated injury to the graft, a careful evidence-based decision is needed to preserve residual renal function. Transplant remains a multidisciplinary speciality, and these patients benefit from combined management involving surgeons, nephrologist, interventional radiologists and pharmacists. In general, most of these grafts can be salvaged by limited radiological and surgical intervention with excellent preservation of graft function.
According to the Trauma Audit and Research Network (TARN), every year 12,500 people die of trauma in United Kingdom (UK) alone and it remains the leading cause of death in children and young adults.[1] According to National health services blood and transplantation (NHSBT) report, released on 7th of April 2017, an increase of 6% is seen in deceased donor kidney transplant compared with the year before.[2] In the last 10 years, 6000 people have died while waiting for solid organ transplantation including 270 children.[3] There is a constant demand for organs and efforts are thus made to further improve transplant numbers. To decrease the gap between demand and supply, higher immunological risk transplants are being attempted. Extended criteria donors and fast track kidney allocations are leading to rise in the kidney transplant activity.[4] Therefore, solid organ transplantation is likely to increase in future and hence we are more likely to come across trauma in transplant recipients than ever before.
Although there are a number of scoring systems to grade traumatic renal injury, none of them describe trauma in transplant recipients. Advanced trauma life support (ATLS) has been shown to improve outcomes in trauma patients.[5] The American Association of Trauma Surgeons (AAST)[6] score has been validated for clinical use[7], and the grade of injury described correlates with the need for intervention, nephrectomy, dialysis and mortality.[8,9,10] Studies involving the validity of advanced trauma life support and Organ injury severity scale for kidney in renal transplant recipients are lacking. Renal transplant recipients are relatively older with poor physiological reserves and multiple co morbidities. According to the18th Annual Report of UK Renal Registry (2015), by the time of start of renal replacement therapy, 49.8% of the patients had one or more comorbidities and this increased to 63.1% in those more than 65 years old. Diabetes mellitus and ischemic heart disease was seen in 36% and 20% respectively.[11] Furthermore; immunosuppression is associated with cardiac toxicity, poor wound healing, an increased incidence of infections and malignancy.[12] In addition, the renal allograft is in a more susceptible position than the native kidneys which are well protected in retro-peritoneum. Therefore, transplant recipients who have had trauma represent a unique cohort of patients requiring specialist management and studies are therefore needed to assess management of trauma and renal allograft in this group of patients.
We present a brief literature review and our experience of two cases of traumatic injuries to allografts in kidney and kidney pancreas transplant recipients, managed at a tertiary care regional trauma center receiving a high volume of trauma patients.[13]
A 46-year-old male with a background of deceased donor transplant 18 years previously, presented as an emergency following a road traffic accident. He was riding a motor bike and was hit at 40 miles per hour. He was successfully resuscitated but noted to have tenderness around the graft and a computerized tomographic (CT) scan revealed an isolated grade III laceration of upper pole of transplant kidney with a peri nephric hematoma (Figure 1). No other injury was identified clinically or radiologically. The patient remained haemodynamically stable and was managed conservatively. A repeat CT scan with contrast 3 days later did not reveal any interval increase in the perinephric collection.
Figure 1. Grade 3 upper pole laceration with a peri-nephric and retroperitoneal haematoma.
He was discharged on the 6th postoperative-day with a stable graft function and his subsequent clinical course remained uneventful, with graft function returning to base line (Figure 2) and no long-term complications at the 6 months follow up.
Figure 2. Renal function tests (Cr umol/L, eGFR-ml/min MDRD) of the patient described in case 1.
A 45 years old male with a simultaneous pancreas kidney transplant done 29 months previously, presented to the emergency department with a history of fall from the second floor. In the emergency department, he was confused, with right sided weakness and Glasgow Coma Scale (GCS) of 14/15. Tenderness was noted in left iliac fossa around the renal allograft. CT scan revealed a large peri nephric hematoma and grade III laceration of transplanted kidney while the rest of the abdomen and transplanted pancreas were unremarkable (Figure 3). The patient was resuscitated and required a transfusion of two units of blood. Shortly thereafter, his GCS dropped and he required intubation.
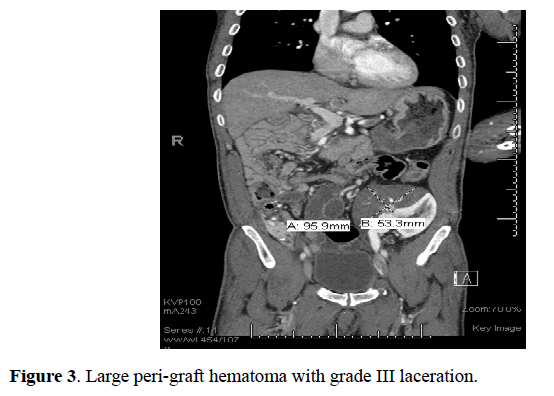
Figure 3. Large peri-graft hematoma with grade III laceration.
Repeat CT scan showed interval increase in size of haematoma with extravasation of contrast suggestive of active bleed.
The case was then discussed between interventional radiologist and transplant surgeons. It was decided to proceed with renal artery angiogram and embolization of bleeding vessel. Angiogram identified active haemorrhage from upper pole cortical vessels which was successfully embolized using micro coils with excellent result. (Super selective embolization). Follow up doppler scan showed good global perfusion with small avascular region in upper pole. The patient had gradual recovery and discharged with stable graft function. There was no complication identified at 6 months follow up and graft function returned to baseline.
A repeat CT scan showed an interval increase in the size of the haematoma with extravasation of contrast, suggestive of active bleeding.
It was decided to proceed with renal artery angiogram and embolization of a bleeding vessel. The angiogram identified an active haemorrhage from upper pole cortical vessels which was successfully embolized using micro coils with good results (Figure 4). A follow-up doppler scan showed good global perfusion with a small avascular region in the upper pole and the patient was discharged after a slow recovery with graft function returning to baseline by 3 weeks (Figure 5). During this period immunosuppression was closely monitored and tacrolimus levels were checked daily during the first week, with dose alteration as required. There were no complications identified at 6 months followup and graft function returned to baseline.
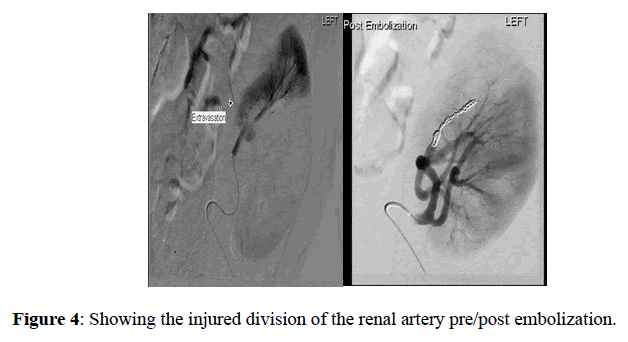
Figure 4. Showing the injured division of the renal artery pre/post embolization.
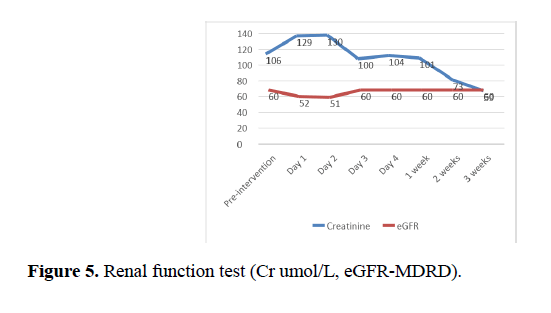
Figure 5. Renal function test (Cr umol/L, eGFR-MDRD).
Renal injuries account for 1-5% of all cases of trauma.[14,15] Depending on the mechanism, they can be classified into blunt or penetrating injuries and the majority is managed conservatively, with only 4.7% requiring a therapeutic laparotomy or angiographic embolization.[16] Therefore, there is an increasing trend towards conservative management of solid organ injuries in trauma. There are two-time periods considered critical with regards to outcome of trauma patients. The 10 platinum minutes in pre-hospital setting and the golden hour in resuscitation department.[17] Patients must be managed according to advanced trauma life support protocols and aggressively resuscitated.
Renal injuries may be missed in up to 22.3% of patients during the initial assessment18 and therefore repeated and regular observations, as well as, investigations such as focused assessment with sonography in trauma (FAST) and CT scans are of paramount importance.
Attention needs to be given to the mechanism of injury which will help identify the severity and complexity of injuries. Polytrauma patients represent only 10% of cases of trauma but mortality is close to 50% in this group which is mostly from intracranial injuries in 40-50%, followed by major hemorrhage in 30-35% and multiorgan failure in 5-10%.[19] Damage control surgery is well established and is applicable to unstable patients unfit for conservative or radiological intervention.[20,21] The type of damage control surgery varies with type and severity of injury and the details of which are beyond the scope of this review.
With regards to urological injury in trauma, certain aspects have to be considered. Preexisting abnormalities in the kidney such as nephrolithiasis, hydronephrosis, accessory renal arteries, hypertension and diabetes need to be taken into consideration.[22] Trauma patients are evaluated soon after injury and serum creatinine may not correspond to the extent of renal damage[23] and hence initial results should be interpreted with caution. There is little correlation between extent of haematuria and renal injury and renal vessel thrombosis. Complete avulsion injury may be seen with no haematuria and correspondingly renal contusions can present with gross hematuria.[23]
Imaging is of critical importance in staging renal trauma, which is then graded using AAST renal injury score. As discussed above, this score has been validated for clinical use and corresponds with need for intervention, nephrectomy, dialysis and mortality.[8,9,10] In trauma patients, FAST scan is used to look for free intra peritoneal or pericardial sac fluid.[24] Ultrasound scan (USS) is not a reliable investigation in renal trauma assessment and has sensitivity of 80-90% in detecting intra-abdominal fluid, but is relatively insensitive for parenchymal and retroperitoneal injuries. Magnetic resonance imaging (MRI) may be considered in stable trauma patients but is costly, time consuming and images are limited by motion artefacts.[25] CT scans have become the diagnostic tool of choice for assessment of renal trauma. Hematuria, hypotension (blood pressure of <90 mmHg) and suspicion of intra-abdominal visceral injury are some of the indications for obtaining a CT scan.[26,27] Arterial and portal venous phases can identify active bleeding and delayed images assess the collecting systems and ureteric continuity.[28] If the patient proceeds to a laparotomy without CT scan and there is a strong suspicion of renal trauma, intra operative single shot intravenous pyelogram is helpful to assess the renal tract.[15]
If the patient is unstable and does not respond to initial resuscitation or deteriorates subsequently, there is a role of damage control surgery. This is usually done in high grade liver and major vascular injuries.[29] The principles of damage control surgery are now well established for severe thoracic, abdominal, extremity and peripheral vascular injuries.[30] Indications for exploration in renal trauma are life threatening haemorrhage, renal pedicle avulsion or pulsatile/expanding hematoma.[31,32] Partial or total nephrectomy is an option in uncontrolled haemorrhage. In isolated renal trauma, overall success rate of conservative management is 90% which falls to 50% in grade V injuries.[33,34]
Grade I injuries are characterized by contusion or sub capsular hematoma without parenchymal laceration. Incidence of these injuries is reported to be approximately 80%. These injuries are managed conservatively.[25]
Grade II injuries are described as non-expanding perinephric hematomas confined to the retroperitoneum or cortical lacerations of <1 cm. There is no involvement of collecting system. Grade III injuries differ from grade II in terms of depth of laceration which is >1 cm. Laceration in grade III injury does not involve the pelvicalyceal system and therefore is not associated with urinary extravasation.[25]
Grade IV injuries involve deep lacerations extending into pelvicalyceal system, renal arteries or veins with either a contained haematoma or segmental infarction. When injuries involve multiple lacerations or renal pedicle, it is categorized as grade V injuries. [23] Grade I-III injuries can be called as low grade and grade IV-V are high grade injuries. It has been observed that in patients with mild to moderate trauma undergoing surgical exploration, risks of complications are twice as compared to patients being managed conservatively for the same grade of injury.[35] For isolated grade IV injuries, conservative management is used more often36 and suspected grade V injuries are an absolute indication for surgical exploration or radiological intervention usually in the form of embolization or coiling.
As discussed earlier, it can be concluded that management of renal trauma is successful in most of the cases with non-operative management, especially in low grade injuries. In addition, with conservative management, incidence of complications is lower when compared with surgical management. However, the ideal method of managing trauma in transplant recipient and to the renal allograft is not clear. Irvine Page in 1939 observed acute hypertension on wrapping animal kidneys with cellophane. It is believed to be caused by peri nephric compression, causing renal ischemia, activation of renin angiotensin, aldosterone pathway which eventually causing kidney damage and hypertension.[37,38] The Page kidney was described for the first time in transplantation in 1976.[39] There have been 30 cases reported in the literature so far of Page kidney, with some related to trauma[40,41] and two cases of allograft losses.[42,43] In transplant recipients, a doppler scan of transplant kidney can show features of compromised renal perfusion such as absent or reversible arterial diastolic flow with significant increase in resistive index coupled with peri graft hematoma.[44] In cases of managing trauma in transplant recipients, it is recommended that the patient is transferred to a transplant unit for specialist care. Hypertension may be managed initially with medications but Page kidney ruled out urgently. Renal doppler scan should be repeated regularly to assess the graft perfusion. In cases of alteration of renal allograft perfusion, evacuation of hematoma should be considered to salvage the graft.[44]
In patients who do not respond to conservative management, there is a role of interventional radiology. Rao et al., concluded that renal artery embolization is effective and minimally invasive for grade III-V blunt trauma injury.[45] There remains a high failure rate of interventional radiology procedures in grade V injuries.[46] It can thus be argued that most but not all renal trauma injuries will respond to interventional radiology techniques. Surgical intervention is associated with high complication rate, however failure to act may result in loss of graft.
Contrary to the belief, studies have shown that trauma patients with previous organ transplants, outcomes are not worse than non-transplanted patients. However, more studies are needed in this regard.45Complications related to renal trauma include urinomas, infections, delayed haemorrhage, pseudoaneurysm, arteriovenous fistula formation and renal insufficiency.46 These potential complications should be actively ruled out after traumatic renal injuries. This will require careful clinical assessment and follow-up imaging.
Renal transplant activity is increasing and we are more likely to see transplant patients presenting with allograft trauma. AAST grading scores are commonly used in renal trauma however; it has not been validated in transplant recipients. Management of trauma in transplant recipients involves a multi-disciplinary approach involving transplant surgeons, nephrologist and interventional radiologist as well as trauma surgeons. Close monitoring of the patients and the graft using USS, ideally in a transplant unit is recommended. Conservative management, radiological intervention and even surgery have its role depending upon the stability of patients, grade of injury and allograft dysfunction. Future studies are needed to develop protocols and grading system to assess the management of traumatic injuries in renal transplant recipients.
None.
Patients have consented for their images to be used for the study and the images are anonymised revealing no personal details.
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.