Case Report - (2021) Volume 0, Issue 0
There is mounting evidence of risk of thrombotic vascular events like stroke, deep vein thrombosis and pulmonary thromboembolism in COVID 19 patients. Risk of stroke increases with advancing age and presence of vascular risk factors. There are cases reported of stroke in young with no known vascular risk factor in COVID 19 patients which is attributed to hypercoagulable state from systemic inflammation, cytokine storm and direct viral induced endothelitis. Biopsy evidence of myocarditis also called as inflammatory cardiomyopathy secondary to SARS-CoV-2 cardio tropism has been recently demonstrated. The two main theories behind are- direct role of ACE2 receptor and a hyper immune response. A final diagnosis of COVID-19 induced myocarditis is seldom made as end myocardial biopsy and cardiac MRI are infrequently done. Hence true incidence of myocarditis in COVID-19 is likely to be higher. Here we are presenting a case report of 26 year old female with two uncommon complications of COVID 19 infection.
COVID 19 • Hypercoagulable • Cytokine storm
World is in middle of pandemic of Coronavirus infection disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV2). There have been approximately 188 million positive cases with 40, 5900 deaths worldwide as of July 14 2021. Although the most common presentation are respiratory symptoms like cough, fever, myalgia, fatigue, shortness of breath, which may deteriorate to acute respiratory distress and multiorgan failure. Reports of neurological manifestations and acute myocardial injury are increasing. Stroke is defined as an abrupt onset of a neurologic deficit that is attributable to a focal vascular cause lasting more than 24 hours [1,2]. A casecontrol analysis of acute stroke protocol imaging done from March to April, 2020 in New York City health system showed that, after adjusting for age, sex, and vascular risk factors, SAS-CoV-2 positivity was independently associated with stroke. Incidence of stroke in COVID-19 patients is 1.74%. Myocarditis-inflammation of the heart muscle occurring as a result of exposure to either discrete external antigens such as viruses, bacteria, parasite, toxins, drugs or internal trigger such as autoimmune activation against self-antigen [3,4]. Most common cause is viral infections. The incidence of myocarditis in COVID 19 infection is estimated as 22 per 100,000. But actual number of cases is much higher [2].We came across a unique and interesting case of young female with large ischemic stroke and concomitant suspected myocarditis.
A 26 years old female with no comorbidities, presented with history of fever, cough and breathlessness since 7 days. RTPCR was done which was positive on 5th day of illness for SARS CoV2. She developed sudden onset blurring of vision, vomiting, weakness of left upper and lower limb and altered sensorium after 3days. On examination, patient was tachypnoeic, with SpO2 of 85% with 15 liters O2, PR-112 bpm (tachycardia), and BP-102/70mmhg. Her GCS was poor (6/15) and paucity of movements on the left side with deviation of angle of mouth to right, pupils 3mm equal and sluggishly reactive to light, plantar extensor on left side. ABG on admission showed type 1 respiratory failure, routine blood investigations showed-neutrophilic leucocytosis (HB-12.3 g/dL, TC-23000/cumm, PLT-4.2 lakhs , Lymphocytes- 3%), procalcitonin-0.5ng/ml, normal -RFT, LFT and serum electrolytes, elevated inflammatory markers (D-dimer-4198 ng/ml ,IL-6 1473 pg/ml, LDH-947 U/L ,CRP-310 mg/L),Imaging shows (Figure 1).
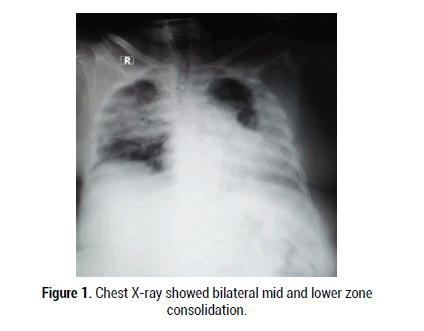
Figure 1:Chest X-ray showed bilateral mid and lower zone consolidation.
MRI and MR angiogram of brain showed large acute infarct in right MCA territory with 6mm midline shift towards left with acute infarct in right cerebellar hemisphere with chronic lacunar infarct in left thalamus with non-visualisation of right ICA and MCA suggesting right ICA thrombosis on MRI (Figure 2). Patient was shifted to ICU and intubated in view of poor GCS. She was started on COVID 19 treatment protocol (approved by ICMR) and received anti-oedema and antiplatelet measures. In view of persistent hypotension put on single inotropic support (Figure 3). Hence 2D-echo was done showed dilated LV global hyperkinesia EF-35%, elevated cardiac markers (TROP I 3658 ng/ml, CKMB- 144 ng/ml, NT pro-BNP-10269 pg/ml). Patient went into sepsis secondary to bronchopneumonia and urinary tract infection (TC-28,600, PLT-28,000, and Procal-7) with multiorgan dysfunction with DIC. (RFTurea- 173, creatinine-2.2 mg/dl, PT/INR-17.2/1.4 s, APTT-42s) was transfused with FFP and platelets. Patient developed gangrene of toes. However patient succumbed to death due to secondary infection.
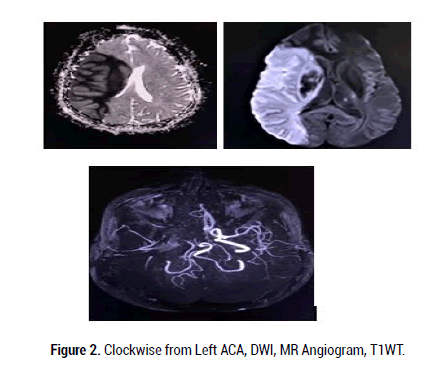
Figure 2: Clockwise from Left ACA, DWI, MR Angiogram, T1WT.
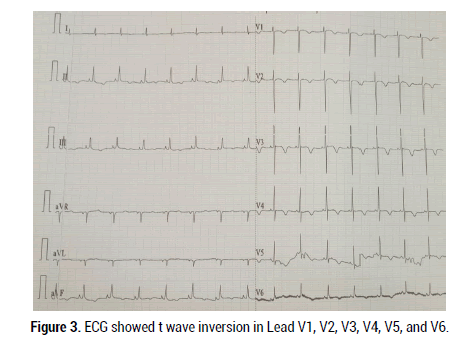
Figure 3: ECG showed t wave inversion in Lead V1, V2, V3, V4, V5, and V6.
The pandemic caused by SARS CoV-2 has caused many deaths. Though respiratory complications are common cause of mortality, there is growing evidence of cardiac and neurological complications leading to death and increased duration of ICU stay. A meta-analysis study showed the incidence of stroke in hospitalized COVID-19 patients is low at 1.74%; the mortality rate is high at 31.76%. In COVID-19 patients, stroke is associated with older age, comorbidities and severe illness. Most patients had at least one COVID-19 symptom like breathlessness, cough, fever or myalgia. About 24.5% were asymptomatic with no COVID-19 symptom. Ischemic stroke (82.8%) was more common than haemorrhagic stroke (17.2%) [5]. The incidence of myocarditis in COVID 19 infection is estimated as 22 per 100,000. But actual number of cases are much higher due to infrequent use of definitive modality like end myocardial biopsy [2].
Mechanism of stroke due to COVID-19 includes
• Coagulopathy-the Systemic Inflammatory Response Syndrome is mediated by COVID-19 virus or viral products. This causes the development of severe coagulopathy, defined as COVID-19 associated coagulopathy characterised by elevation of blood coagulation markers (D-dimers, fibrinogen), rise of inflammatory markers (PT, aPTT), and mild thrombocytopenia, and leads to increased clot formation.
• Endothelitis-inflammation of endothelial cells due to direct virus mediated injury.
• Unopposed angiotensin 2 action due to lack of ACE2 mediated counterbalance causing lung injury and endothelial dysfunction in brain and heart.
• Cytokine storm- promotes atherosclerosis, plaque rupture, and superimposed thrombosis [6].
Mechanism of myocarditis in COVID-19 includes
• immune-mediated, both innate and acquired immune responses contribute to myocardial injury with the sequelae of dilated cardiomyopathy
• autoimmune-mediated, in response to the release of cryptic antigens from cardiac myocytes that are normally secluded from the immune system following virus-mediated injury
• Direct virus-induced- SARS-CoV-2 may invade cardiac myocytes using their surface ACE2 receptors and may cause direct cellular damage [7].
A case report by Avvantaqqiato, et al. Ischemic Stroke in a 29-Year- Old female patient with COVID-19 without vascular risk factors. Stroke was involving territories of right anterior and middle cerebral arteries. Similar case was reported Quenzer, et al. where 32 year old male had acute cerebellar infarct with COVID-19 [7]. Both patients had increased WBC counts, lymphopenia, increased inflammatory markers like ddimer, LDH and CRP. A case of clinical fulminant myocarditis was reported by et al in a 63 year old COVID-19 patient who had raised IL-6, CRP, and lymphopenia with features of myocarditis [8].
Our patient was a 26 years young female with no known vascular risk factors with COVID-19. Presenting with symptoms of COVID-19 and stroke. Laboratory parameters showed lymphopenia, increased inflammatory markers like IL-6, LDH - evidence of cytokine storm. Increased dimer, prolonged PT, aPTT and thrombocytopenia - evidence of coagulopathy. Increased cardiac biomarkers like troponin I, NT pro BNP, ECG showing t wave inversion , Echo showing dilated LV with reduced fraction and MRI brain showing acute infract in two different region with thrombosis indicates COVID-19 induced systemic inflammation has lead to cytokine storm and coagulopathy causing wide spread thrombosis with ischemic stroke and probable myocarditis . Other tests for defect in coagulation like Protein C and S, factor, Von Will brand factor, ANA screening, Antiphospholipid antibody, homocysteine and vitamin B12 were normal.
All patients with COVID-19 should undergo routine investigations irrespective of the age, severity and comorbidities as there is increasing incidence of neurological and cardiovascular complications even without vascular risk factors. This might help in early detection of virus induced systemic inflammatory response and cytokine storm and started on appropriate treatment. When a patient presents with stroke without respiratory complaints COVID-19 should also be tested to prevent exposure to uninfected individuals and to start appropriate treatment.
Citation: Varsha V, et al. A Case of Stroke and Suspected Inflammatory Cardiomyopathy in Young Female with COVID-19. Med Rep Case Stud, 2021, 06(S6), 035-036
Received: 01-Dec-2021 Published: 22-Dec-2021
Copyright: © 2021 Varsha V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.