Case Report - (2023) Volume 9, Issue 2
Giant Cell Carcinoma of the Lung (GCCL) is a rare histological form of poorly differentiated non-small cell lung cancer, which is classified as a subtype of pulmonary sarcomatoid carcinomas. Here we report the case of known Multidrug Resistant Tuberculosis (MDR-PTB) patient presented with left lung mass diagnosed as giant cell carcinoma of lung with skin metastasis as a suboccipital swelling. GCCL is a poorly differentiated non-small cell lung cancer. GCCL has exceptionally aggressive characteristics and its prognosis is much poorer than other NSCLCs. Although cutaneous metastasis from the lung is rare, it must be ruled out in patients with suspicious skin lesions, smoking history, or lung cancer.
Sarcomatoid carcinoma • Giant cell carcinoma of the lung • Multidrug resistant tuberculosis • Skin metatstasis
Lung cancer is the most common cancer worldwide and is still responsible for the most cancer deaths according to the World Health Organization. The 2015 World Health Organization (WHO) classification of lung tumors should be the foundation for lung cancer classification [1, 2]. In contrast to previous classification systems, the 2015 WHO classification relies to a greater extent on immunohistochemical characterization in addition to light microscopy, allowing for subtyping that more judiciously guides treatment strategy and predicts clinical course.
According to the 2015 WHO classification of lung tumors, Giant Cell Carcinoma of the Lung (GCCL) is classified as a subtype of Pulmonary Sarcomatoid Carcinomas (PSCs). Sarcomatoid carcinoma is a broad term that represents a heterogeneous group of Non-Small Cell Lung Carcinomas (NSCLCs, meaning they have a malignant epithelial component) that also contain a component of true sarcoma or are composed in part or completely of sarcoma like elements. Sarcomatoid carcinomas are rare, comprising less than 1 percent of all lung cancers [3].
A 48 years old male, presented with complaints of left sided chest pain and hoarseness of voice since 4 months. Patient also complained of loss of appetite and weight since 3 months associated with malaise and dry cough. Patient was a known case of MDR-PTB since 20 months and was on anti-tubercular treatment.
Patient was a smoker with a 30 pack year’s history, non-alcoholic.
On general physical examination clubbing and pallor was present. A well circumscribed reddish swelling was present in the suboccipital region, non-tender, semisolid, approx 5 cm × 6 cm in size (Figure 1). Patient was afebrile and vitals were stable.
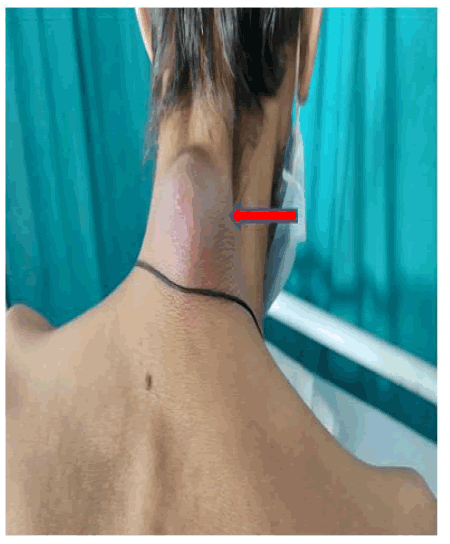
Figure 1: A well circumscribed reddish swelling was present in the suboccipital region, non-tender, semisolid, approx 5 cm Ã? 6 cm in size.
On chest examination, chest movement appears to be decreased on left side, intensity of breath sounds decreased on left side with no added sounds present. All other routine investigations were within normal limit. Chest radiograph shows a homogenous opacity in left upper zone (Figure 2).
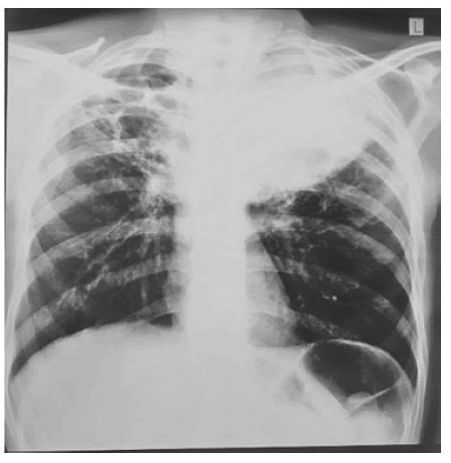
Figure 2: CHEST radiograph showing a well-defined homogenous opacity in left upper zone.
Contrast Enhanced CT chest (CECT) showing heterogenous lobulated solid mass lesion in left upper lobe with patchy areas of necrosis (Figure 3) and right upper lobe fibrocavitatory changes (Figure 4). No mediastinal or hilar lymphadenopathy was noted.

Figure 3: CECT chest showing heterogeneous mass lesion in left upper lobe with patchy areas of necrosis.
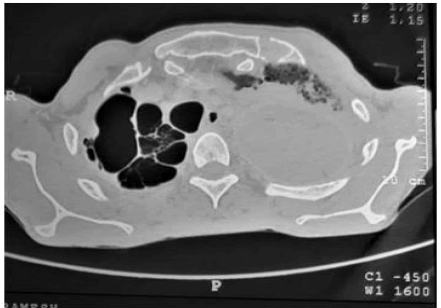
Figure 4: Showing right upper lobe fibrocavitatory disease suggestive of old infective lesions.
Fiberoptic bronchoscopy was done showing left vocal cord palsy and exophytic growth in left upper lobe, biopsy was taken from growth and sent for histopathology examination, but report was inconclusive. USG guided FNAC done from left upper lobe mass lesion. Cytopathology examination shows sheets of malignant epithelial cells with high N/C ratio having hyperchromatic pleomorphic nucleus. Overall cytomorphology was suggestive of malignant adenocarcinoma.
On the other hand, FNAC done from suboccipital swelling, sample was sent for microscopic, CBNAAT and cytopathological examination. Microscopy and CBNAAT was negative for tuberculosis. Cytopathology smears show atypical epithelial cells singly lying with nuclear enlargement, hyperchromasia and irregular membrane, many giant cells also seen on a background of neutrophils, overall suggestive of atypical cells. Excisional biopsy of suboccipital swelling was done to further confirm the diagnosis of metastasis and sample was sent for Histopathological Examination (HPE), which was in favour of poorly differentiated malignant neoplasm (Figure 5).
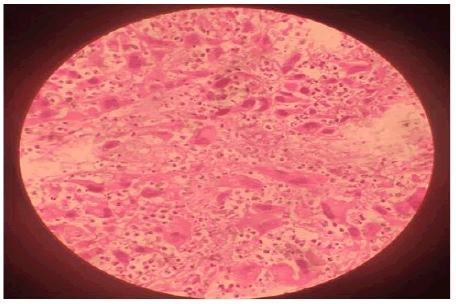
Figure 5: H and E staining reveals large cell with bizzare nuclei arranged in clusters. Abundant eosinophilic cytoplasm with tumor giant cells are seen.
Immunohistochemical study shows extremely bizzare, large tumor cells with numerous multinucleated cells, stroma shows numerous neutrophils. The cells also show emperipolesis and cell cell features and was positive for PanCK, CK7, Calretinin and CD10. All these features are consistent with diagnosis of Giant Cell Carcinoma of lung, a rare entity.
Giant cell carcinoma, a rare malignant form of large cell lung carcinoma, a subtype of PSCs. The GCCL incidence was much lower than other four PSC subtypes [4]. GCCL comprised about 0.3%–0.4% of primary lung cancers, with an incidence of about three new cases per million persons per year [5]. Like other Non-Small Cell Lung Cancers (NSCLCs), GCCL can invade in any lung lobes, but it is observed much more frequently in the upper lobes and always at periphery [6].
GCCL is essentially undifferentiated and usually appears as a bulky necrotic mass, having no distinct architectural pattern. Under microscope, tumor cells are frequently multinucleated and may contain polymorphonuclear leukocytes in their cytoplasm, cells have an abundant, thick and well demarcated cytoplasm. The nucleus is oval or irregular and centrifugal. Multinucleated giant cells are observed more often than uninuclear cells. Large, bizarre tumor cells are not specific to any one histologic category and can be seen in otherwise typical squamous cell and adenocarcinomas. The term giant cell carcinoma is restricted to those tumors in which bizarre pleomorphic giant cells (greater than 40 microns) comprise almost the entirety of the neoplastic population.
Another specific feature known about this malignancy is the presence of a phenomenon called emperipolesis: Collections of polymorphonuclear leukocytes within the giant cells, apparently phagocytosing cytoplasmic content which was also present in our case.
GCCL is a poorly differentiated non-small-cell lung cancer with early metastasis through lymph and blood circulation to the brain, bone, adrenal gland and liver, similar to other NSCLCs, but uncommon metastasis to the gastrointestinal tract, kidney and heart is reported constantly. The incidence of lung cancer with metastases to the skin varies between 1%–12%, with the highest incidence seen in men. Although cutaneous metastases from lung cancer are rare, but it should be ruled out in patients with suspicious skin lesion, smoking history. As our patient was also a known case of MDR-PTB, suspicion of reactivation of tuberculosis was also high. So our primary aim was to rule out tuberculosis from suspected skin lesion, which came out to be negative.
For limited stage GCCL, surgical resection is an effective treatment and provides adequate local control. However, most cases of GCCL are quite advanced at the time of diagnosis (50% of patients present with metastasis situation),13,18 and even after surgery, most patients experience tumor recurrence or death within 16 months–18 months.
Platinum based chemotherapy has been used to treat GCCL by most clinicians, but plenty of studies demonstrate the poor response of GCCL to chemotherapy in general. We need more treatment options like molecular targeted therapy for patients with GCCL.
It has exceptionally aggressive characteristics and its prognosis is much poorer than other NSCLCs. Although complete tumor excision and chemotherapy are often adopted in clinical use, the tumor seems to have a poor response to any currently known treatment modality, including platinum based chemotherapy and radiotherapy. But early and precise diagnosis helps in better management and prognosis of the disease
Nil.
Citation: Chaudhary K, et al. "A Rare Case of Giant Cell Carcinoma of Lung Presenting with Skin Metastasis". Oncol Cancer Case Rep, 2023, 9 (2), 1-3.
Received: 19-Sep-2022, Manuscript No. OCCRS-22-75086; Editor assigned: 22-Sep-2022, Pre QC No. OCCRS-22-75086 (PQ); Reviewed: 07-Oct-2022, QC No. OCCRS-22-75086; Revised: 14-Feb-2023, Manuscript No. OCCRS-22-75086 (R); Published: 21-Feb-2023, DOI: 10.37532/2471-8556.23.9.2.1-3
Copyright: © 2023 Chaudhary K,This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.