Case Report - (2021) Volume 6, Issue 6
Background: Birt–Hogg–Dubé (BHD) syndrome is a rare, genetic disorder, inherited by autosomal dominant disorder. It is caused by a germline mutation in the follicular gene (17p11.2). It is characterized by benign skin lesions, renal tumours, and pulmonary cysts. We report the case of a 52‐ year‐old man who presented at the dermatology department of 401 Military Hospital of Athens with multiple papules on face, scalp and neck. He reported a history of renal cancer and nephrectomy. Additional genomic sequencing confirmed a diagnosis of BHD syndrome.
Synonyms: Fibrofolliculomas with trichodiscomas and acrochordons, Hornstein-Knickenberg syndrome, Birt Hogg Dube syndrome
Objective: To present a case story and propose a surveillance strategy for patients and family members.
Case study: The probed was a 52-year-old Greek man who presented at the Dermatology department with multiple asymptomatic, soft skin‐coloured papules on his face, neck and trunk. Histopathologically, the papules revealed a fibrofolliculoma.
Results: Clinical exome panel sequencing analysis of peripheral blood of the probed detected the FLCN mutation, which was a nucleoside insert c1285dupC in exon 11.
Conclusion: Birt-Hogg-Dube Syndrome is a rare inherited syndrome. The disorder should be considered in patients with skin manifestations in coexistence with spontaneous pneumothorax or cystic lung disease and renal cancers. Early diagnosis is very important in order to subject patients to systematic screening for renal cancers. A surveillance protocol/strategy for these patients are proposed.
Birt hogg dube syndrome • Hornstein-knickenberg syndrome • Diagnosis
Birt-Hogg-Dube syndrome is a rare, complex, genetic disorder, inherited by autosomal dominant disorder, caused by mutations in the Follicular Gene (FLCN). It was firstly described by Birt, Hogg and Dube in 1977 [1]. The main characteristics of the disorder are cutaneous manifestations, lung involvement and high predisposition to renal cancer. Skin lesions (fibrofolliculomas, acrochordons, angiofibromas, oral papules, cutaneous collagenomas, and epidermal cysts) usually appear after the age of 20 years old. The most common of these, fibrofolliculomas, appear as domeshaped skin-coloured or whitish papules on face, neck and trunk. They are asymptomatic. Lung involvement appears with lung cysts or spontaneous pneumothorax, usually multiple episodes, seen exceptionally rarely in patients younger than 40 years. In terms of renal cancer predisposition, many patients are reported to have renal cancer, unilateral, bilateral or multifocal, and the mean age of diagnosis is 50,7 years old [2]. The most common type of the tumours is chromophore, oncocytoma or oncolytic hybrid, and less often, clears cell renal carcinoma. Patients with BHD syndrome may also have other tumours, benign or malignant (colorectal polypus and cancer, thyroid gland nodules and parotid tumours), but no causal relationship has been reported. According to the BHD Foundation, reported families with this syndrome worldwide in 2017 were about 663, mostly reported in USA and Japan.
Birt-Hogg-Dube syndrome is a rare, complex, genetic disorder, inherited by autosomal dominant disorder, caused by mutations in the Follicular Gene (FLCN). It was firstly described by Birt, Hogg and Dube in 1977 [1]. The main characteristics of the disorder are cutaneous manifestations, lung involvement and high predisposition to renal cancer. Skin lesions (fibrofolliculomas, acrochordons, angiofibromas, oral papules, cutaneous collagenomas, and epidermal cysts) usually appear after the age of 20 years old. The most common of these, fibrofolliculomas, appear as domeshaped skin-coloured or whitish papules on face, neck and trunk. They are asymptomatic. Lung involvement appears with lung cysts or spontaneous pneumothorax, usually multiple episodes, seen exceptionally rarely in patients younger than 40 years. In terms of renal cancer predisposition, many patients are reported to have renal cancer, unilateral, bilateral or multifocal, and the mean age of diagnosis is 50,7 years old [2]. The most common type of the tumours is chromophore, oncocytoma or oncolytic hybrid, and less often, clears cell renal carcinoma. Patients with BHD syndrome may also have other tumours, benign or malignant (colorectal polypus and cancer, thyroid gland nodules and parotid tumours), but no causal relationship has been reported. According to the BHD Foundation, reported families with this syndrome worldwide in 2017 were about 663, mostly reported in USA and Japan.
A 52-year-old Greek non-smoker man, with a history of radical right nephrectomy due to chromophore renal cell carcinoma with no adjuvant therapy (2016) (Figure 1) and Diabetes Mellitus Type II (since 2016), presented in October 2020 at the dermatology department of 401 General Military Hospital of Athens. On clinical examination, we reported multiple skincoloured and whitish papules on face, scalp, neck and chest and acrochordonlike lesions (Figures 2 and 3). The lesions appeared when the patient was about 40 years old, and was the reason of the consultation. We performed a biopsy of a typical papule on the face, which revealed a fibrofolliculoma/ trichodiscoma. Further check was performed. No pathologic evidence found in basic blood count, biochemical blood tests. In chest imaging by computed tomography, two pulmonary cysts were found in left lung (Figure 4). Due to the patient’s history of renal tumour and skin manifestations, he was referred to diagnostic genetic testing, which revealed a c.1285dupC exon 11 mutation (heterozygous). He was diagnosed with Birt-Hogg-Dube syndrome as he fulfils two major and one minor criterion (one major or two minor criteria is needed for establishing the diagnosis) [3]. He was referred also to genetic consultation. Upon checking family history, we found that his mother died of breast cancer and his father died from pancreatic cancer, but there was not known history of spontaneous pneumothorax or skin manifestations in his family members. The patient has three children, with no history of skin, pulmonary or renal manifestations, who were also referred to presymptomatic genetic testing. The oldest one, 26 years old, has also Birt-Hogg-Dube syndrome. Our patient was also referred to the gastroenterology department for having his first screening colonoscopy, because of his age. Two polypus were found, removed and biopsied. Both of them were benign lesions.
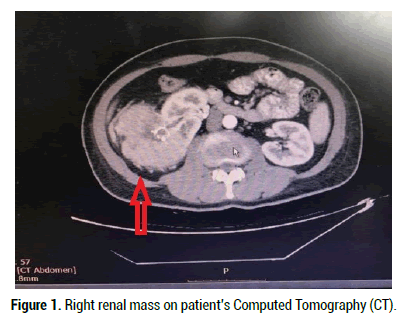
Figure 1: Right renal mass on patient’s Computed Tomography (CT).

Figure 2: Papules on patient’s face.
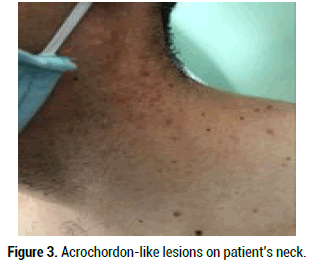
Figure 3: Acrochordon-like lesions on patient’s neck.
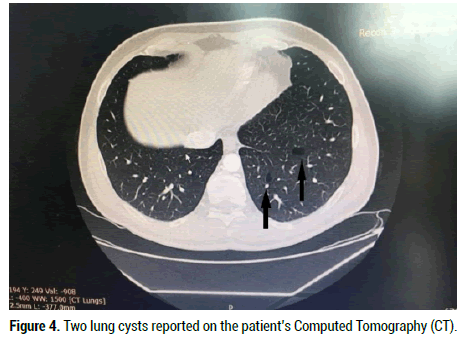
Figure 4: Two lung cysts reported on the patient’s Computed Tomography (CT).
Diagnosis of BHD syndrome is very important, so patients are included in screening programs, even though it is a rare syndrome. Referral should be considered for any individual with a personal history of or first-degree relative with (i) ≥ 5 Birt–Hogg–Dubé–associated facial or truncal papules; (ii) earlyonset (<50 years old), bilateral or multifocal clear cell renal carcinoma; (iii) renal cancers with Birt–Hogg–Dubé histology (chromophore, oncocytoma, or oncolytic hybrid); or (iv) lung cysts associated with multiple spontaneous pneumothoraxes [4,5]. Diagnosis could be made by the European BHDS consortium criteria [3]. Upon diagnosis of BHDS, the patients should undergo examination of the skin for fibrofolliculomas, CT imaging of the thorax for lung cysts, abdominal MR or CT imaging for renal tumors as well as genetic screening for pathogenic FLCN mutations. Treatment of the syndrome manifestations is needed in some cases. The skin lesions are benign, and no therapy or follow-up is needed [6]. It is made only for cosmetic purpose, by surgical and laser procedures, but lesions often recur over time [7-9]. Topical treatment of fibrofolliculomas with the mTOR inhibitor rapamycin, in a double-blinded placebo-controlled randomized split-face study showed no effect [10]. The treatment of pneumothorax in BHDS is similar to the treatment of pneumothorax of other etiologist [11]. Because of the high recurrence rate of pneumothorax, it is recommended to consider pleurodesis after the first episode of spontaneous pneumothorax [12]. Renal cell carcinoma is one of the most dreaded complications, so diagnosis and management is very important. Patients with no renal tumour at first diagnosis of the syndrome should be examined by urologist annually. According to the European Academy of Urology, diagnosis or surveillance of renal masses should be made by CT or by MRI in younger patient for the risk of accumulative radiation. It is recommended that tumours smaller than 7 cm, limited to the kidney, should be treated by a partial nephrectomy (T1 tumours). Tumors bigger than 7 cm, limited to the kidney, should be treated by radical nephrectomy (T2 tumours). Our patient was treated by radical nephrectomy. Follow-up is also very important for the risk of recurrent renal cell carcinoma [13]. As there is no surveillance recommendation by consensus yet, the writers propose follow-up guidelines for individuals with Birt-Hogg-Dube syndrome. It is proposed that, as general measures, patients should quit smoking [14], maintain a normal body weight and a normal blood pressure. As air travel and diving was found to increase pneumothorax risk, patients should avoid these (in case of long-distance flight, it is proposed that the patients undergo a lung CT before travelling) [15]. Pneumococcal vaccination and annual influenza vaccination should be strongly encouraged in patients with BHD. Furthermore, use of nephrotoxic medication should be avoided in patients with nephrectomy. Annual chest x-ray or computed tomography is not recommended as a routine screening for these individuals, in order to avoid cumulative radiation exposure. Although, a chest x-ray or a computed tomography is recommended immediately in individuals with symptoms or signs of pneumothorax. A dermatologic exam is not recommended as a routine exam for individuals with fibrofolliculomas, as they are benign tumors, but a full body examination every 6 or 12 months is recommended for possible risk of melanoma. It is not well established yet whether individuals with BHD syndrome are in higher risk for melanoma compared to general population, but numerous studies have observed melanomas in individuals with this syndrome [16-18]. With respect to renal surveillance, a pelvic MRI should be offered at the age of 20 years old [3,19,20] as a first examination and then every two years, as most of the renal cancers tend to have slowprogression. In patients with suspicious renal tumors, an annual pelvic MRI should be considered. Renal ultrasound could be considered as a surveillance in the interval between two MRIs, but not as a screening method, as it is not reliable on tumors <3 cm. As 56% of the patients develop bilateral tumors and 65%-77% develops multiple tumors, patients already operated for one renal tumour [21-23], should continue monitoring for this crucial complication. Surveillance by CT should be avoided for the risk of accumulative radiation. In some studies, it has been observed that patients with BHD syndrome develop parotid tumors (parotid oncocytoma, Warthin parotid tumors and pleomorphic adenoma) [16,24,25]. An annual examination for signs of swelling or pain of parotid glands should be considered. Thyroid cancer, nodules, cysts have been also reported on these patients [16,26-28]. It is recommended that the patients have a thyroid ultrasound per year for early identification of thyroid manifestations. The increased risk for colon cancer is suggested in individuals with BHD syndrome, but it is not confirmed yet [29,30]. On patients with a family history of colon cancer, it is recommended that they have a colonoscopy 10 years before the age of onset of colorectal cancer in affected relative. When no family history of colorectal cancer is present, first colonoscopy should be considered at age of 40 years old. A study, by Nahorski, et al. found that 10 BHD patients out of the 149 assessed had CRC or colorectal polyps. This was linked to the c.1285dupC exon 11 mutation; suggesting patients with this particular mutation are more at risk of developing CRC. This mutation was revealed in our patients’ genetic test [31].
Many other tumors and manifestations have been reported in patients with BHD syndrome. Surveillance is not generally recommended in these patients, but it is recommended that the patients visit a healthcare specialist for evaluation of a new manifestation. Finally, genetic testing of offspring’s of the probed should be offered. Genetic counselling and surveillance should be proposed in all the affected patients.
Citation: Katsarou S, et al. Birt-Hogg-Dube Syndrome: A Case Report of Family Inheritance in Greece and Suggested Follow-up Guidelines. Med Rep Case Stud, 2021, 06(6), 228
Received: 04-Nov-2021 Published: 25-Nov-2021, DOI: 10.35248/2572-5130.21.6.228
Copyright: © 2021 Katsarou S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO