Research Article - (2021) Volume 11, Issue 5
Background: The contact with the health care within 48 hours and before end of the first week would be the most effective strategy for the mothers and their babies to reduce deaths. Globally, most maternal and new-born death occurs within this period. However, it is yet neglected; little attention and an effort have been paid by health care providers and policy makers in low income countries. Hence the aim of this study was to determine early postnatal service utilization and associated factors among women, who gave birth in the last 12 months prior to March, 2020.
Methods and participants: Community based cross-sectional study design was conducted on 612 mothers by using multistage sampling method from March 1-30, 2020. Interviewer administered pre-tested questionnaire which is adopted from the Ethiopian Demographic and Health Survey, World health organization and from different literatures was used to collect data. The collected data was entered into EpiData version 3.1 and then exported into SPSS window version 21 for analysis. In bivariate logistic regression variables with p-value less than 0.25 were selected for multiple logistic regression analyses and in multiple logistic regression analysis p value less than 0.05 was used to declare statistical significance. Finally adjusted odds ratio was used to measure strength of association.
Results: The prevalence of early postnatal care services utilization among postnatal mothers was 24.9%. Number of live birth [(AOR: 4.16, 95% CI: 1.6- 10)], Mode of delivery [(AOR: 3, 95% CI: 1.4-7.8)], previous history of early postnatal care utilization [(AOR: 1.8, 95% CI: 1.01-3.375)], complications at labor and delivery [(AOR: 2.3, 95% CI: 1.314-4.27)], Hours to reach health facility [(AOR: 2.4, 95% CI: 1.4-4.)], and Knowledge of respondents [(AOR: 1.8, 95% CI: 1.1-3)] were significantly associated factors with early postnatal care utilization.
Conclusion: in this study early postnatal service utilization was low. Number of birth, Mode of delivery, early postnatal care utilization in the previous delivery, Faced complications during labor and delivery, Distance/time took to arrive health facility on foot and knowledge of mothers were factors affecting early postnatal care utilization.
Lemmo district, Early postnatal care, Utilization, Mothers
The contact with the health care within 48 hours and before end of the first week would be the most effective strategy for the mothers and their babies to reduce deaths. Maternal mortality occurs from risks attributable to pregnancy and child birth as well as poor availability and quality of maternal health services. The most common cause of maternal mortality in sub Saharan countries include haemorrhage (34%), sepsis or infection (10%), hypertensive disorder (9%), HIV and AIDS (6%), other direct causes (5%) and other indirect causes contribute approximately 17% [1,2].
“If birth is at facility, the mothers and new-borns should receive PNC during the first 24 hours after birth. If birth is at home, the first postnatal contact should be as early as possible within 24 hours of birth. Three additional postnatal contacts are recommended for all mothers and newborns, on day 3(48-72hours), between 7-14 days, and six weeks after birth’’, and extra contacts for those LBW/mothers living with HIV. Also home visits in the first week after birth are recommended for care of the mother and new-born [2,3].
Early Postnatal care is very important period, because of it can bring a change to the health and life chances of mothers and their babies as well as it can also reduce maternal and new-born mortality and enhance survival, particularly it helps to early detection and management of postpartum complications that happen following delivery [4-7].
The fact that the majority of maternal and new-born deaths occur during the first week of the postnatal period. Regarding to postnatal care service utilization, countries taken different strategies to increase uptake of PNC utilization. One of the strategies was developing universal coverage. Ethiopia government accepts this strategy to improve PNC service utilization. Many health extensions workers were arranged in the past few years and linking health centres with health posts [8-10].
A large number of birth in low income countries still occur at home without the assistance of skilled birth attendants, the fact that 18 million women in Africa currently give birth at home due to challenges for planning and implementing PNC for mothers and their newborns. therefore, every year in Africa, at least 125,000 women and 870,000 newborns die in the first week after birth [11-14].
Despite the benefits of EPNC, most new-born and mothers do not receive EPNC services from a skilled health care provider after delivery in sub Saharan Africa country [4,7,15]. EPNC is neglected, a little attention and an effort have been paid by health care providers and policy makers over the country and maternal mortality is still high. Also the previous published researches in Ethiopia at different regions were not focused on EPNC utilization, rather focused on PNC service utilization in general. This indicates that the factors associated with utilization of EPNC is still need strong attention to be investigated so, as to improve its utilization and similar study is lacking in the study setting. This study is, therefore, aimed to assess Early Postnatal Care utilization and associated factors among mothers who gave birth in the last twelve months in lemmo district.
Study Setting and Design
A community based cross sectional study was conducted in Lemmo district. Lemmo district is found in Hadiya Zone Southern, Ethiopia and it is 232 km away from Addis Ababa
According to the District Annual report in 2019, lemmo distric has a total of 30 kebeles (4 urban and 26 rural) which had a total population of 150,706 from which 76,060 were females. There were 5576 postnatal mothers under twelve months. The district has 7 health centers, 35 health post, 6 private clinics and 5 drug stores. According to 2019 report of lemmo health office, there were 177 all types of health professionals and 66 health extension workers in the districtThis study was conducted in Lemmo district from March 1-30, 2020.
Population
Source of population
All mothers who gave birth within the past tweleve months in lemmo district, southern Ethiopia.
Study population
Randomly selected mothers who gave birth in the past tweleve months and found in selected kebeles during the study period.
Criteria
Inclusion criteria
All mothers who gave birth within the past twelve months prior to the study period and resident at least for six months in lemmo district during data collection time was included in this study.
Exclusion criteria
All Mothers who have under twelve months old child but unable to respond because who are not mentally and physical capable of being interviewed during data collection time.
Sample Size Determination
The sample size was determined by using a single-population proportion formula, by taking prevalence of 23.7% which is the prevalence of Early Postnatal Care service Utilization [6]. Considering the following assumption, 5% margin of error and 95% confidence level (Z = 1:96). The calculated sample size was 278. Taking nonresponse rate of 10% and design effect of 2 because a multistage sampling technique was employed, the total sample size was 612.
Sampling Procedure
We have used multi-stage sampling technique and simple random technique to select 30% kebeles from 26 rural and 4 urban kebeles. Hence, 8 kebeles from the rural and 1(Jawe) kelebe from the urban had been selected by lottory method. The sample size was proportionaly distributed to the nine selected kebeles based on their population. In each selected kebeles, a list of mothers who gave birth in the last twelve months and their full addresses was be enumerated by using family folders of each household from health post data. Finally, the respondents which was included in the study from each kebele was identified by using simple random sampling technique based on the sampling frame obtained from kebele health extension workers registration books. For household with more than one mother having under twelve-month child, one of the mothers was selected using lottery method (Table 1).
| kebeles | # of mothers | % (weight) | Sample |
|---|---|---|---|
| Jewe | 186 | 0.122 | 75 |
| Lareba | 168 | 0.111 | 68 |
| Lissana | 143 | 0.094 | 58 |
| Orma | 171 | 0.114 | 69 |
| Kalisha | 153 | 0.1 | 61 |
| Masibira | 132 | 0.086 | 53 |
| Kidiga | 179 | 0.117 | 72 |
| Shurmo | 191 | 0.125 | 77 |
| Bobicho | 197 | 0.129 | 79 |
| 1520 | 612 |
Table 1. Proportionally allocated sample size for selected kebeless.
Data collection tools
Data was collected by using an interviewer administered structured questionnaire which was adopted from the EDHS (Ethiopian Demographic and Health Survey), WHO and by reviewing different literatures.
Data collection procedures
Explanation was given on the purpose of the study and importance of their involvement. Then Respondents who was volunteer mothers are interviewing face to face using structured and pre-tested questionnaires by going to household level. The data was collected by trained 10 diploma nurses and midwifery’s and supervised by 2 BSC holder nurses who were fluent in local languages hadiyisa and Amharic.
Early postnatal care utilization
In this study mothers and new born babies those who had at least one Early postnatal care check-up for the current delivery by health workers and health extension workers from 2 days up to 7 days following delivery [6,15].
Antenatal care utilized
Those mothers who visited ANC clinic at least one check-up by the health care provider during her current pregnancy [11].
Good knowledge
Those Mothers who were capable of answering mean and above out of 8 knowledge questions [1,6,16].
Data Quality Control
The questionnaire was first prepared in English and translated to Amharic and hadiyisa languages. The questionnaire was pre-tested on 5% of sample size in the district which were not part of the study kebeles. The findings and experiences from the pre-test were used in modifying data collection tool. Data collectors and supervisors were recruited. The reason why we chose nurses or midwifery’s for data collection was to give health education at the end of data collection.
Training was given for data collectors and supervisors about the objective of the study, confidentiality of information, respondent’s right, maintain privacy techniques of interviewing prior to data collection. Completeness of questionnaire was checked by principal investigator and supervisors on daily basis. Finally, multivariate analysis was run in the binary logistic model to control the confounding factors.
Methods of Data Analysis
Data were entered into EpiData v3.1, exported to SPSS version 21 and cleaned to check for completeness and missing values. Principal component analysis (PCA) was be used to estimate wealth indices of households. Earlier to use PCA, its assumptions were checked. I.e. Bartlett's Test of Sphericity was significant, Sampling adequacy with Kaiser-MeyerOlkin measure of sampling adequacy was >0.5 and Varimax rotation was used to minimize cross loading of items on to many factors.
Descriptive statistical analysis such as: -simple frequency, measure of central tendency, and measure of variability was used to describe the characteristics of participants such as: - socio-demographic, obstetric factors, knowledge of mothers about EPNC, and health facility and care provider factors. The results were presented using frequencies, tables, sentences and figures.
Bivariate analysis was done to see the association between each independent variable and the outcome variable by using binary logistic regression. All variables with p < 0.25 in the bivariate analysis were included in the final model of multivariate in order to control all possible confounders. The direction and strength of statistical association was measured by adjusted odds ratio with 95% CI. The goodness of fit was tested by Hosmer- Lomeshow statistic test and it was not significant. I.e. it is a good fit. Finally, in this study variables whose p-value < 0.05 was considered as statistically significant association.
Ethical Considerations
Ethical clearance was obtained from Haramaya University, college of Health and medical sciences, Institutional Health Research Ethics Review Committee (HU-IHRERC).
Permission letter was obtained from the Hadiya Zone Health Department and lemmo woreda health office. Participants were informed about the objectives of the study, and informed consent for participation was obtained from individual participants. Finally, participants were informed that they had full right not to participate in the study
For those mothers whose age is less than 18 years the permission was asked from her parents/ guardian. Privacy and cultural norms was respected. At the end of the data collection, the data collectors gave health education about EPNC utilization, any PNC and advantage of ANC.
Socio-Demographic Characteristics of Study Participants
Out of 612 sample size 603 respondents were interviewed which yielded response rate of 98.5%. The mean age of the respondents was 29.19 and SD± 5.63 years. Almost half of respondents were protestant religion followers and majority were Hadiya by ethnicity which were found 310(51.4%) and 483(80.1%) respectively. Regarding place of residency one urban and eight rural kebeles, 75(12.4%) and 528 (87.6%) respectively. Regarding to educational status, 379(62.9%) of mothers had no formal education. Regarding to occupational status, 302(50.1%) of mothers were housewife. Almost all study participants were married 553(91.7%), and 238(39.5%) households were middle percentile group of wealth index (Table 2).
| Variable | Frequency | Percent (%) |
|---|---|---|
| Age of respondents | ||
| 15-19 | 33 | 5.5 |
| 20-24 | 70 | 11.6 |
| 25-29 | 200 | 33.2 |
| 30-34 | 245 | 40.6 |
| 35-49 | 55 | 9.1 |
| Religion | ||
| Protestant | 310 | 51.4 |
| Orthodox | 156 | 25.9 |
| Muslim | 137 | 22.7 |
| Ethnicity | ||
| Hadiya | 483 | 80.1 |
| Kambata | 49 | 8.1 |
| Slite | 38 | 6.3 |
| Others* | 33 | 5.5* |
| Place of residency | ||
| Rural | 528 | 87.6 |
| Urban | 75 | 12.4 |
| Marital status | ||
| Married | 553 | 91.7 |
| Others** | 50 | 8.3** |
| Maternal educational status | ||
| No formal education | 379 | 62.9 |
| Primary school (1-8) | 124 | 20.6 |
| Secondary school(9-12) | 57 | 9.5 |
| College and above | 43 | 7.1 |
| Husband educational status | ||
| No formal education | 298 | 49.4 |
| Primary school (1-8) | 152 | 25.2 |
| Secondary school (9-12) | 91 | 15.1 |
| College and above | 62 | 10.3 |
| Mother occupation | ||
| Housewife | 302 | 50.1 |
| Farmer | 174 | 28.9 |
| Daily labourer | 81 | 13.4 |
| Others*** | 46 | 7.6*** |
| Husband occupation | ||
| Farmer | 396 | 65.7 |
| Daily labourer | 91 | 15.1 |
| Merchant | 77 | 12.8 |
| Employed | 39 | 6.5 |
| (Household) | ||
| Wealth index | ||
| Lowest | 200 | 33.2 |
| Middle | 238 | 39.5 |
| Highest | 165 | 27.4 |
Table 2. Socio-demographic characteristics among postnatal mothers in lemmo district southern Ethiopia, March 2020 (N=603).
Obstetric Characteristics
Out of all the respondents, 552(91.5%) had no history of abortion and 558(92.5%) reported planned last pregnancy. Regarding number of live birth 320(53.1%) had given, four to six. Large proportion, 511(84.7%) of mother had ANC follow up. Large proportion, 511(84.7%) of mothers had ANC follow up, out of those who had ANC follow up 149(24.7%), 200(33.2%), 98(16.3%) , and 64(10.6%) of respondents visited one time, two times, three times, and four times respectively.
Out of mothers who gave birth before, 89(14.8%) had utilized early postnatal care in previous delivery. Totally 105(17.4%) reported experience of labour and delivery related complication, of them 39(6.5%) experienced prolonged labour. Also mothers who had developed complications after delivery were totally 128(21.2%) from these 28(4.7%), 24(4.0%), 20(3.3%), 16(2.7%), 15(2.5%), 14(2.3%), and 11(1.8%) had faced heavy bleeding, high grade fever, severe headache, blurring vision, severe abdominal pain, offensive vaginal discharge, and redness and pain on breast respectively (Table 3).
| Variables | Frequency | Percent (%) |
|---|---|---|
| History of abortion | ||
| Yes | 51 | 8.5 |
| No | 552 | 91.5 |
| Pregnancy planed/wanted | ||
| Yes | 558 | 92.5 |
| No | 45 | 7.5 |
| Number of live birth | ||
| 3-Jan | 85 | 14.1 |
| 6-Apr | 320 | 53.1 |
| >6 | 198 | 32.8 |
| ANC visit | ||
| Yes | 511 | 84.7 |
| No | 92 | 15.3 |
| Previous history of EPNC utilization | ||
| Yes | 89 | 14.8 |
| No | 514 | 85.2 |
| Complication at time of labour and delivery | ||
| Yes | 105 | 17.4 |
| No | 498 | 82.6 |
| Faced complications at time of labour and delivery (N= 105) | ||
| Prolonged labour | 39 | 6.5 |
| Fetal distress | 35 | 5.8 |
| PIH(pre-eclampsia/eclampsia | 31 | 5.1 |
| Faced Complication after delivery | ||
| Yes | 128 | 21.2 |
| No | 475 | 78.8 |
Table 3. Frequency of obstetric Characteristics of respondents in Lemmo District, Hadiya Zone, southern Ethiopia, March 2020, (N=603).
Mode of Delivery
Majority of respondents, 515(85.4%) were delivered spontaneously vaginal delivery. Forty Five (7.5%) and forty three (7.1%) were delivered by instrumental delivery and obstetrics caesarean section respectively.
Health Care Providers’ and Facility services Related Characteristics
From the total respondents 411(68.2%) of participants took one hour and more to arrive to the nearest health facility and majority of 421(69.8%) of respondents had no access to transportation. For 137(22.7%) of mothers had got information/advice from health professional about early PNC check-up. Regarding to place of delivery 429(71.1%) of respondents gave births their last child in governmental health facility. Mothers who gave birth in health facility were totally 566(93.9%) out of these 418(69.3%) had PNC appointments and visits, on the other hand 124 (20.6%), 68(11.3%), 82(13.6%) and 144(23.9%) had been given postnatal appointments and visited within 24 hours, within 2-3 days, within 6-7 days and on six weeks respectively. For 302(50.1%) of mothers had advised on postpartum and new-born complications after delivery from health professionals (Table 4).
| Variables | Frequency | Percent (%) |
|---|---|---|
| Distance | ||
| < one hour / <5km | 192 | 31.8 |
| ≥ one hour/ ≥ 5km | 411 | 68.2 |
| Access to transportation | ||
| Yes | 182 | 30.2 |
| No | 421 | 69.8 |
| Information/advice | ||
| Yes | 137 | 22.7 |
| No | 466 | 77.3 |
| Place of delivery | ||
| Governmental Health facility | 429 | 71.1 |
| Private clinic/hospital | 82 | 13.6 |
| Health post | 55 | 9.1 |
| Home | 37 | 6.1 |
| Delivery attendants | ||
| Health professionals | 566 | 93.9 |
| Others* | 37 | 6.1 |
| Having appointment for EPNC utilization From health profession (N=566) | ||
| Yes | 418 | 69.3 |
| No | 148 | 24.5 |
| Time of appointment for EPNC (N=418) | ||
| Within 24 hours | 124 | 20.6 |
| Within 2-3 days | 68 | 11.3 |
| Within 6-7 days | 82 | 13.6 |
| On six weeks | 144 | 23.9 |
Table 4. Health care providers' characteristics and utilization of early postnatal care in lemmo district, southern, Ethiopia, march 2020 (N=603).
Knowledge of Respondents About Early PNC Utilization
Majority of the respondents 468(77.6%) have poor knowledge towards early postnatal care utilization.
Prevalence of Early Postnatal Care Utilization
The prevalence of early postnatal care utilization was 150 (24.9%), among these, 68 (11.3%) of participants had got within 2-3 days following delivery, whereas 82 (13.6%) had got within 6-7 days of postpartum period (Figure 1).
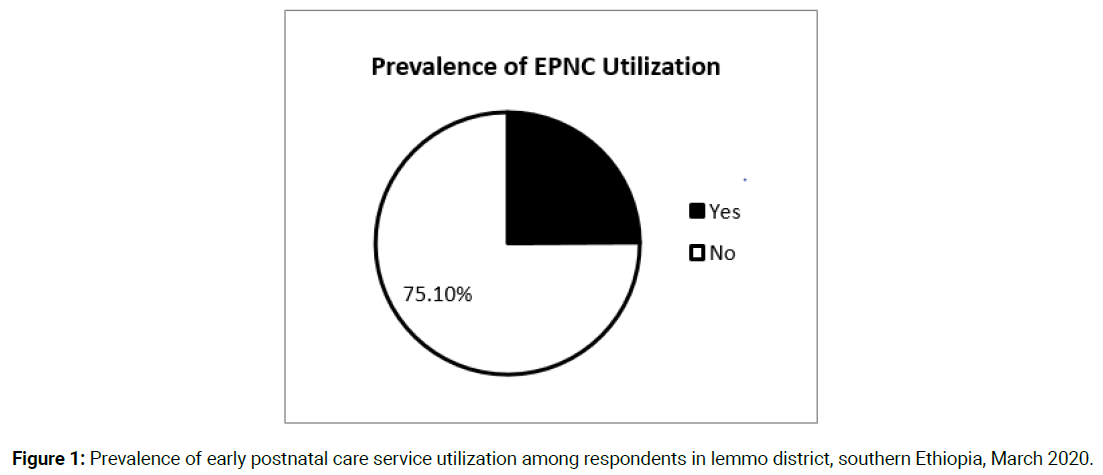
Figure 1. Prevalence of early postnatal care service utilization among respondents in lemmo district, southern Ethiopia, March 2020.
Types of Services Provided during Early Postnatal Period Percentage
Most of mothers had received immunization services followed by advising on exclusive breast feeding (Table 5).
| Variables | Frequency | Percent (%) |
|---|---|---|
| Provision of immunization | ||
| Yes | 139 | 23.1 |
| No | 11 | 1.8 |
| Advising on exclusive breast feeding | ||
| Yes | 115 | 19.1 |
| No | 35 | 5.8 |
| Provision of family planning | ||
| Yes | 114 | 18.9 |
| No | 36 | 6 |
| Advising on danger signs after delivery | ||
| Yes | 103 | 17.1 |
| No | 47 | 7.8 |
| Advising on nutrition | ||
| Yes | 84 | 13.9 |
| No | 66 | 11 |
| Physical examination for mother | ||
| Yes | 80 | 13.3 |
| No | 70 | 11.6 |
| Advising on hygiene | ||
| Yes | 79 | 13.1 |
| No | 71 | 11.8 |
| Physical examination for baby | ||
| Yes | 67 | 11.1 |
| No | 83 | 13.8 |
Table 5. Type of EPNC services provided for mothers after delivery, in Lemmo District, Hadiya Zone, southern Ethiopia, March 2020 (N = 150).
Reasons for Not Having Early Postnatal Care Utilization Percentage
The main reasons stated by mothers for not using early postnatal care utilization were culturally there is belief that until 7 days of delivery mothers should not go away from home 210(35%), health professionals were not good at care giving 207 (34%), waiting for falling off baby’s cord stump 194(32%), lack of guardians for my children171(28%) lack of time165(27%), lack information (advice) 155(26%), to have enough energy 148(24%), Waiting the service kill the time141(23%) and the Pregnancy was unplanned 45(8%).
Factors Associated with Early Postnatal Care Utilization among Postnatal Mothers
In simple logistic regression analysis the following variables were candidates for multivariable logistic regression analysis or p-value <25%. Place of residence, Marital status, Educational status of mothers, Wealth index of the respondents, Number of live birth, ANC follow up, previous history of early PNC utilization, Mode of delivery, Place of delivery, Complications faced at time of labour and delivery, Complications faced after delivery, Hours to reach nearest health facility, Access of transportation, Information about early PNC utilization and Knowledge of mothers about early PNC service utilization.
Results of the Multivariable Analysis
Number of live birth, Previous history of EPNC utilization, Mode of delivery, Faced complications at the time of labour and delivery, Hours to reach nearest health facility, and Knowledge of respondents were significantly associated factors with early postnatal care services utilization in multivariable logistic regression analysis.
Mothers who gave birth more than six child were 4.2 times more likely to utilize early postnatal care services than those mothers who gave less than four children [(AOR:4.163, 95% CI: 1.674-10.353)]. Mothers who delivered by caesarean section were 3.3 times more likely to utilize early postnatal care services utilization than mothers who delivered by spontaneous vaginal delivery [(AOR: 3.254, 95% CI: 1.359-7.790)]. Mothers with experience of early postnatal care for previous child were 1.85 times more likely to utilize early postnatal care than mothers with had no experience in previous delivery [(AOR: 1.845, 95% CI: 1.009-3.375)].
Mothers who had complication during labor and delivery were 2.3 times more likely to utilize early postnatal care as compared to those who had no complication during labor and delivery [(AOR: 2.369, 95% CI: 1.314-4.271)]. The study finding showed mothers who travelled for less than one hour on foot to arrive at nearest health facility were 2.4 times more likely to utilize early postnatal care utilization than mothers who travelled for one hour and more [(AOR: 2.431, 95% CI: 1.451-4.071)]. Mothers with good knowledge level about early postnatal care utilization were 1.8 times more likely to utilize early postnatal care utilization than those with poor level of knowledge about EPNC [(AOR: 1.821, 95% CI: 1.065-3.112)] (Table 6).
| Variable | EPNC utilization | Adjusted OR(95%CI) | p-value | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| Number of birth | |||||
| 3-Jan | 8 (9.4%) | 77 (90.6%) | 1 | 0.003 | |
| 6-Apr | 54 (27.3%) | 144 (72.7%) 232 (72.5%) | 3.778 (0.895-9.099) |
0.002 | |
| >6 | 88 (27.5%) | 4.163 (1.674-10.352) |
|||
| Mode of delivery | |||||
| Normal Delivery(SVD) | 98 (19%) | 417 (81%) | 1 | 0.106 | |
| Instrumental delivery | 25 (55.6%) | 20 (44.4%) | 1.948 (0.867-4.373) |
0.008 | |
| Caesarean Section | 27 (62.8%) | 16 (37.2%) | 3.254 (1.359-7.790) |
||
| EPNC utilization in the previous delivery | No 39 (43.8%) | 50 (56.2%) | 1 | 0.047 | |
| Yes 111 (21.6%) | 403 (78.4%) | 1.845 (1.009-3.375) |
|||
| Ever faced Complications at time of labor and delivery | No 93 (18.7%) | 405 (81.3%) | 1 | 0.004 | |
| Yes 57 (54.3%) | 48 (45.7%) | 2.369 (1.314-4.271) |
|||
| Hours to reach nearest health facility | |||||
| ≥ one hour/ ≥ 5km | 71 (17.3%) | 340 (82.7%) 113 (58.9%) |
1 | 0.001 | |
| < one hour / <5km | 79 (41.1%) | 2.431 (1.451-4.071) |
|||
| Knowledge of respondents | |||||
| Poor knowledge | 95 (20.3%) | 373 (79.7%) 80 (59.3%) | 1 | 0.028 | |
| Good knowledge | 55 (40.7%) | 1.821 (1.065-3.112) |
|||
Table 6. Multivariable Logistic Regression Analysis showing factors associated with Early PNC Service Utilization in Lemmo Woreda, Southern Ethiopia, March 2020.
In this current study, overall prevalence of early postnatal care services utilization among postnatal mothers was 24.9% (95% CI=21.9-28.2), from which (11.3% within 2-3 days and 13.6% within 6-7days).
Evidence from the present study indicated that early postnatal care utilization was 24.9%. This finding is comparable with the study done at Malaga district Sidama zone and Aseko district, Arsi Zone, Ethiopia was 22.5% and 23.7% respectively. This difference might be attributed to the time gap between the studies, socio-demographic differences and health service accessibility [6,15].
However, this study also showed that early postnatal care utilization in the district to be significantly higher than the study conducted soroti district, eastern Uganda in 2015, where only 15.4% of mothers used EPNC utilization. In addition the result of current study indicates the services utilization of EPNC to be higher than EDHS in 2016, study results that show only 17% mothers PNC within 2 days. Also current study is higher than study conducted in Dembecha, northwest Ethiopia, which was 0.8% in 2015 [5,17]. The possible reason for the difference might be accessibility of health services, time difference and high community mobilization through different mechanisms like women development army.
Mothers who gave birth more than six were 4.2 times odds of more likely to utilize early postnatal care utilization than those mothers with less than four children. This finding is inconsistency with study conducted in Addis Ababa, Ethiopia [9]. This inconsistency might be due to as the number of birth increases the chance of giving birth in health institution also increases that mothers seeking obstetric care for their delivery because they believe that they are at risk of developing obstetric and new born complications. This makes mothers go to health institution and they get EPNC.
Mothers with experience of early PNC for previous child were 1.85 times more likely to utilize early postnatal care services than mothers with had no experience. This finding was consistent with study conducted in Malaga district, South region and Aseko district Ormia region, Ethiopia [6,15]. This may be explained by experienced mothers may had better opportunity to get information/advice provision on the importance of early postnatal care service follow up during previous child from health care providers.
Mothers who delivered by caeserean section were 3.3 times more likely to utilize EPNC services than mothers who delivered by spontaneous vaginal delivery. This study is consistent with study conducted in Debre markos town Northwestern, Ethiopia [14]. This might be due to fear of complication and exposure to health care services to prevent further complications and increase health care seeking behaviour and they stay more times in the health facility.
Mothers who had developed complication during labour and delivery were 2.3 times more likely to utilize EPNC services when compared to those who had not developed any complication during labour and delivery. This study is consistent with study was conducted in Debre markos town, north western and Mertule Mariam District Northwest Ethiopia [1,14]. This was probably the mothers who had complication at a time of delivery were consulted by health care providers immediately after delivery and advised on the necessity of EPNC utilization. In addition to this, the health personnel put complicated mothers while giving birth in a special corner of care to prevent complications and they want to check mother weather they had improved or not, this makes the mothers go to health institutions.
With regard to distance of home from health facility, the study showed that mothers who travelled for less than one hour on foot to arrive at nearest health facility were 2.4 times more likely to utilize EPNC services than mothers who travelled for one and more than one hour. This finding is consistent with study conducted in Dembecha district of Amhare region, Aseko district of Ormia region and Malaga district South region, Ethiopia [6,15,17]. This may be explained due to the reason that having nearby health facility increases access of health information and reduces distance barriers leading to better utilization.
Mothers who have good knowledge were 1.8 times more likely to utilize early postnatal care services than those who have poor knowledge. This finding is consistent with the study conducted in Bangladesh and diga district, east wollega zone, wester Ethiopia [16]. This is due to the fact that mothers with good knowledge about early postnatal care would have perception of benefits of EPNC than those who did not have, so they seek EPNC because they know the advantage of taking EPNC for their postpartum health. The other possible explanation to this might be due to the fact that knowledge about EPNC enhances positive health belief and perception which in turn increases health seeking behaviour. In other word, this can be explained by the fact that knowledge about EPNC is an important factor in motivating mothers and their families to uptake health care services at the earliest opportunity in prevention, early detection and managing postpartum complications.
The findings of this study show that early postnatal care service utilization in the study area was low. This implies that nearly a quarter of the participants were using early PNC utilization. Number of birth, Mode of delivery, EPNC utilization in the previous delivery, Faced complications during labor and delivery, Distance/time took to arrive nearest health facility on foot and knowledge of mothers were associated factors with early postnatal care service utilization that motivated the mothers to have EPNC utilization.
Since it is twelve months by which postpartum period was completed, it might be subjected to recall bias.
Alemu T: had contributed a lot on conception, acquisition of data, analysis and interpretation of data, and Demena M, Assebe T, RadM, Belay Erchafo had revised the paper from proposal development to manuscript preparation. All authors read and approved the final version of manuscript.
Our special thanks to data collectors, supervisors, study participants and Hadiya Zone Health Department, Woreda health office and health posts. We would also like to thank Haramaya University.
Citation: Alemu, T., et al. Early Postnatal Care Utilization and Associated Factors Among Mothers Who Gave Birth in The Last Twelve Months in Lemmo District, Hadiya Zone, Southern Ethiopia. Prim Health Care, 2021, 11(5), 380.
Received: 28-Apr-2021 Published: 29-May-2021, DOI: 10.35248/2167-1079.21.11.380
Copyright: © 2021 Tekeba Alemu, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.