Case Series - (2022) Volume 7, Issue 1
Conventional radiation therapy has been progressively replaced by Fractionated Stereotactic Radiotherapy (FSRT) and single fraction radiosurgery for dealing with benign intracranial lesions. Treatment options for these tumors include surgical resection, fractionated External Beam Radiation Therapy (EBRT), Stereotactic Radiosurgery (SRS), and/or Stereotactic Body Radiation Therapy (SBRT). Purpose of our study is to investigate the safety and efficacy of SBRT in a series of two patients with benign intracranial tumors treated at our radiotherapy department this last year. The first case is a meningioma and the second a tympanic paraganglioma.
Benign cerebral tumors • Radiotherapy • Stereotactic body radiation therapy • External beam radiation therapy
Surgery is usually considered the treatment of choice for intracranial benign tumors as a gross total resection may assure long-term local control [1,2]. Nevertheless, the surgical iatrogenic effects frequently observed, which are increasingly unacceptable for a benign tumor, the growing importance of quality of life, the better knowledge of the natural history of the tumor, improvement of techniques and introduction of new irradiation modalities explain why radiotherapy now, once again, constitutes an essential treatment option [3,4]. In symptomatic de novo or recurrent/residual patients in which surgery is not an option or in patients with documented neuroradiological residual tumor growth, radiation therapy is an option to control the disease. Although conventional fractionated radiation therapy has been historically effective in controlling these types of tumors [5-7], over the last 2 decades FSRT and single fraction radiosurgery have progressively replaced conventional radiotherapy in these clinical situations. This change is due to technologic advances in both the precise delivery techniques and the accurate, rapid dose calculation methods [8,9]. The aim of this paper is to rapport the experience of the radiotherapy department of national oncologic institute in treatment of benign intracranial tumors with SBRT through two observations with a literature review.
Observation 1
D.F, 69 years old, female with a medical history of thyroidectomy, no notion of previous radiation therapy. She complained of headache and dizziness for 6 months with a progressive evolution. A cerebral computed scan revealed a process of the left cerebellum measuring 20/20/18 mm with a mass effect and small edema without any hydrocephaly in favor of meningioma. Then a magnetic resonance imaging was performed during her hospitalization at neurosurgery and showed a left occipital meningioma with mass effect on cerebellum and left transverse sinus thrombosis. The decision of the multidisciplinary consultation meeting was SBRT. At radiotherapy consultation, the patient was in good general condition and had a totally normal neurological examination. Then, she was comfortably positioned on the CT simulation table and a custom mask was fabricated. A thin-slice high resolution CT with intravenous contrast was then obtained while the patient was immobilized. The acquired images were then transferred to the treatment planning workstation. The tumor volume and surrounding critical structures were manually contoured. The volume of the GTV (Gross Target Volume) was 2,27 cc and the PTV (Planning Target volume) consisted of an automatic margin of 3 mm around the GTV (Figure 1). Dose volume histograms were calculated for the tumor volume and nearby critical structures and were utilized to select the optimal treatment plan. The prescribed dose was 21 Gy in 3 fractions to the 100% isodose line. The 100% of our PTV received 99, 69 % of the prescribed dose. The physician used three Arcs ballistic. At 3 months following treatment, the patient had no functional complaints and radiographic follow-up was based on thin-slice gadoliniumenhanced skull base MRI was obtained. Tumor response was assessed and classified as stable disease. Another MRI is planned at 6 months.
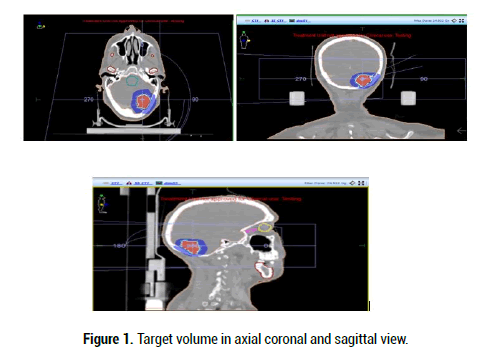
Figure 1: Target volume in axial coronal and sagittal view.
Observation 2
E.A, 44 years old, female, complaining of pulsating tinnitus on her left ear, otorrhagia and ipsilateral hearing loss for 1 year. Otoscopy showed a purple hemorrhagic tumor budding in the external ear canal. Audiometry diagnosed mild sensorineural hearing loss of 20 dB. CT scan and MRI showed a tumor of the external left ear canal ensuring 21/10/10 mm extended to petrous pyramid with lysis of the ipsilateral carotid duct in favor of tympaojugular glomus classified grade C of Fish. The surgery was difficult considering the anatomy complexity of the area and the great risk of hemorrhage. The SBRT treatment plan used 4 Arcs ballistics and the prescribed dose was 25 Gy in 5 fractions to respect cochlea dose constraint. To note that the GTV measured 2 cc and the 100% of the PTV received 99, 08% of the prescribed dose, while respecting the dose constraint of cochlea who received 24 Gy us a dose maximum (Figure 2). The follow up at 3 months found a clear clinical improvement with disappearance of all complaints. We don’t note ay toxicity of treatment. The MRI showed a tumor regression 13/6/5 mm versus 21/10/10 and a control audiometry is planned.
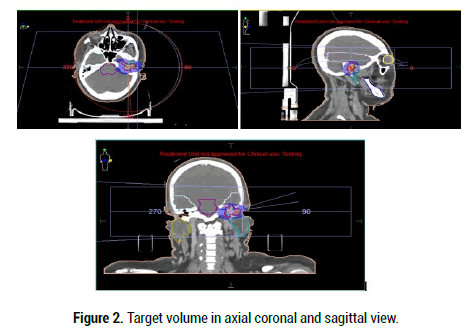
Figure 2: Target volume in axial coronal and sagittal view.
Meningioma is the most common benign, primary, intracranial tumor [10]. Historically, first line treatment for meningioma requiring intervention has been resection with the role of Radiation Therapy (RT) dependent upon World Health Organization (WHO) histopathological tumor grade. Resection or RT alone has similar outcomes for grade I lesions [11], and choice of modality depends on safety of resection, patient comorbidities, and patient preference. Adjuvant RT is controversial for Grade II lesions but recommended for Grade III lesions due to improved rates of local control with addition of RT [12-18]. A systematic review of outcomes with SRS for meningioma found mean 5 and 10-year actuarial LC rates of 91% and 87.6% in the literature, respectively [19]. Tumor control with SRS is high, but improving patient quality of life by improving rates of post-radiation symptoms in patients receiving stereotactic radiosurgery is also a priority. Studies have shown that SRS has baseline overall rates of perilesional edema ranging from 2.5%-37% [20]. A summary of LC, OS, and toxicity data from studies of FSRT demonstrated 2-year and 5-year LC rates ranging from 85%-100% and 83%- 89%, respectively [21-25]. Paragangliomas are rare hyper vascular low-grade malignancies of neural crest origin (chief cells) arising within the autonomic nervous system. They are believed to store and secrete catecholamine in response to neuronal or chemical stimuli. Glomus tumors are the most common tumor of the middle ear and the second most common tumor of the temporal bone. These tumors (sometimes referred to as chemodectomas) occur predominantly in women, are more common on the left side, and are metacentric in 3 to 10% of sporadic cases [26]. Although surgery has historically been used as the primary treatment modality for SBP, radiation therapy has also been used as a definitive treatment of these tumors without operative risks. Multiple series and metaanalyses have suggested that radiation therapy has similar Local Control (LC) as surgery. Stereotactic radiotherapy has been increasingly used for the treatment of SBP. A meta-analysis including Gamma Knife (Elektra, Stockholm, Sweden) and LINAC (linear accelerator)-based stereotactic radiotherapy showed tumor control rates to range from 80 to 100% with favorable toxicity profile [27,28]. Patients were treated to a dose of 14-25 Gray (Gy) in a single fraction or 18-25 Gy in three fractions [29-31]. To minimize potential late cochlear and cranial nerve toxicity from single-fraction Gamma Knife radiosurgery, a five-fraction approach has been developed.
While surgery remains a treatment option for benign intracranial tumors, our modest experience and a literature review of retrospective series suggest that stereotactic radiotherapy is an attractive treatment modality. It has similar local control rates and a more favorable toxicity profile.
Google Scholar Cross Ref
Citation: Benlemlih M, et al. Fractionated Stereotactic Radiotherapy for Benign Intracranial Tumors: About Two Cases and Literature Review. Med Rep Case Stud, 2021, 06(S6), 030-031
Received: 14-Dec-2021 Editor assigned: 30-Mar-2022 Revised: 31-Mar-2022 Published: 04-Jan-2022
Copyright: © 2021 Benlemlih M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO