Research Article - (2021) Volume 7, Issue 11
Background: One of the most health problems in adolescent is obesity. Obesity is correlated with impairments on risky decision making and food addiction. Standard bio-psycho-socials treatments have many limitations that cause to relapses in diet by obese participants. Base on this factors, this study investigate Acceptance and commitment treatment (as emerging and promising field) for risky decision making, food addiction severity index, and BMI in adolescent girls with overweight and obesity.
Material and Methods: 60 obese girls were selected to attend in this study using convenient sampling method. The participants were randomly classified into two groups of control and experimental groups. In experimental group acceptance and commitment therapy was applied and in control group psycho-education. Every participant receive specific diet therapy. For collecting data the PC version of IOWA gambling task, Yale food addiction scale, and BMI index were utilized. The mean and standard deviation of descriptive statistics were used for illustrating and depicting the data. Also, in order to analyze the data, ANOVA with repeated measure and chi-squared tests were employed.
Results: The mean score of risky decision making in experiment group was significantly higher than control group (P<0.05) during post-test and follow up. In addition, food addiction rate was significantly lower in experiment group than control group through post-test and follow up. The results of repeated measures ANOVA for comparison of the changes of BMI showed that in posttest and follow up, the mean score of this variable in the experimental group was significantly higher than the control group (p˂0.001)
Conclusion: Acceptance and commitment therapy can significantly lead to improvement of risky decision making system and food addiction in with overweight and obesity. Also this treatment can decline BMI index in obese and overweight girls.
Acceptance and Commitment Therapy • BMI • Addiction
Obesity is a Multidimensional problem. In addition to the wide bio-psychosocial risks for the person and the society, it is accompanied by many other diseases such as diabetes and cardiovascular diseases [1,2].
One of the groups vulnerable to obesity is the adolescents [3]. According to the WHO assessments in 2016, averagely 18% of the world’s children and adolescents of 5-19 years old are affected by overweight and obesity. This percentage is equal to the prevalence rate of overweight and obesity in Iran [4,5]. According to the reports, 77% of the obese children will become obese adults. This situation increases the risk of being affected by chronic diseases such as type 2 diabetes, increased blood pressure, increased cholesterol, cardiovascular diseases, atherosclerosis, orthopedic diseases, some cancers, and consequently early death [6,7]. Furthermore, most of the dietary habits and patterns are formed in childhood and remain for the rest of life; this fact raises the importance of investigating and treating obese adolescents [4].
In spite of the psychological and medical interventions for treating obesity, the improvement rate is still low in these people and the results are contradictory [7,8]. One of the causes of slip in drug adherence in diseases (and slip in addition) is disordered decision making system. In fact, deficiency of risky decision making system makes the person take long term risks for small and instantaneous rewards (high-calorie foods, drugs, etc.) and lose the benefits gained from the long term abstinence [9,10]. This structure has been widely investigated in the area of addiction. Nevertheless, in addition to the above mentioned concepts, recent studies suggest that there are shared patterns of neural activity among the obese and addicted people. Therefore, deficiency of risky decision making system in obese people is one of the causes of slip and impulsive binge eating in these people which prevents the preservation of the treatment results [11].
A structure consistent with risky decision is food addiction. Recent studies in the area of food addiction suggest that special types of food can create addictive eating behaviors (loss of control, craving) in people, and it leads to psychological and physical injuries [12]. The recent studies investigating the eating patterns have found similar patterns between impulsive eating behaviors and alcohol abuse [13,14]. Approving the issue of food addiction, MRI studies shown that the signs of visual food and using high-calorie foods activate the reward-related brain circuits in human in a similar way to drug abuse [14]. So, in order to achieve a sustainable intervention and preserve the changes resulted from the treatment, food addiction should be paid special attention.
Pharmacotherapy can be used as a way of reducing weight in people with overweight and obesity [15]. The role of pharmacotherapy in treating obese people is so challenging; because effectiveness of drugs in treating these people is sometimes contradictory [15,16]. There are clinical trials studies suggesting that as the use of drugs continues, the weight loss procedure becomes slow and by cutting down the use of drugs, most patients return to their previous weight [15-17]. However, a way of promoting the effectiveness and sustainability of the drug effects is exercise; but the role of exercise in achieving this purpose is not so significant [17]. Therefore, there are still challenges in pharmacotherapy and mobility in people with overweight and obesity.
The solution for resolving the deficiencies of pharmacotherapy and mere exercise is the promising choice of psychological treatment. As overweight and obesity begin and continue by bio-psychosocial dimensions, psychological treatments should be widely paid attention in this area [17].
The most common psychotherapy used for treating overweight and obesity so far is cognitive-behavioral therapy (CBT). The goals of this treatment include helping the patients to accept the achieved weight loss, encouraging them to accept weight stability rather than weight loss as their goal, and helping the patients to learn behavioral skills and cognitive responses needed for a successful weight control [17,18]. In spite of efficiency of this approach in different areas, it is accompanied by some limit. For example, this approach is only focused on the thought content; whereas, clinical experiences suggest that most of the people who are affected by psychological disorders and emotion regulation problems cannot recognize extreme cognitive distortion [19]. Furthermore, although rationalization might be advantageous, studies suggest that due to lack of attention control training, there is a high rate of rumination recurrence in cognitive-behavioral therapy [20]. Therefore, traditional psychological interventions are not usually useful for these patients. The other constraint of cognitive-behavioral therapy is the limitation of each protocol to a specific problem or disorder, and a single protocol has not the capacity of simultaneous treatment of several separate symptoms and deficiencies; whereas as stated above, comorbidity of impulsiveness and food addiction is observed in obese adolescents [21]. Many studies have shown that this treatment is not useful for comorbidity symptoms [21,22].
Through mindfulness training and focusing on changing the person’s relation with internal experiences such as thoughts, impulses, and emotions rather than directly changing these experiences, acceptance and commitment therapy increases adjustability and acceptance of emotions, decrease impulsive behaviors, and improves decision making system [23,24]. The model of this treatment includes six major processes all of which are focused on flexibility. These six processes include acceptance, defusion, committed action, determination of goals and values, self-ascontext, and contacting the present moment [19]. Mindfulness training is an important component of acceptance commitment therapy. These trainings play a fundamental role in regulation of prefrontal cortex function. Also by affecting the emotion regulation system, they can play an effective role in reduction of craving, adjustment of decision making system deficiencies, and consequently reduction of food addiction [20,25- 27]. The commitment component of this treatment seeks for recognition of the emotions and thoughts. Recognition is not about to approve that these thoughts are true; rather, it seeks for breaking the vicious cycle of impulsive action based on emotions. People learn that the existence of positive and negative emotions does not require acting based on them. This non-judgmental awareness changes the person’s relation with thoughts and emotions. As a result, when facing with decision making situation, rather than trying to strictly controlling these emotions or denying themselves, people try to make a proper decision by regulating their emotions [28].
Nevertheless, so far no study has investigated the effect of acceptance commitment therapy on these structures to improve the methods of treating obesity under a clinical trial. In addition, studies performed on the effect of acceptance and commitment therapy on obesity have been faced with many constraints. Due to the bio-psychosocial nature of obesity, this study investigates the effectiveness of integrated acceptance and commitment therapy and therapeutic regimen on risky decision making, food addiction severity index, and BMI in adolescent girls with overweight and obesity as a high-risk group.
Research design
The present study is a controlled randomized clinical trial including pretest, posttest, and follow up. The research population includes the adolescent girls referring to nutrition clinics and medical offices of nutrition experts. All the adolescent girls who had referred to nutrition clinics of Kashan in the period of April 20th, 2017-June 21st, 2017 (108 people) were checked by the specialists in terms of the inclusion and exclusion criteria. Then, out of the people having inclusion criteria (93 adolescent girls), 50 people were selected by random number table. Afterwards, based on “random allocation rule”, 25 people were assigned to the experimental group and the remaining subjects (25 people) were assigned to the control group. The experimental group received acceptance and commitment therapy and the control group received psycho-education individual advice for 12 weekly sessions. It should be mentioned that both groups received therapeutic regimen under supervision of a nutrition specialist. During the interventions, the subjects of both the experimental and the control groups were randomly assigned to 4 or 6-people blocks and received group therapy. The patients were aware of participating in a research and the research goal i.e. investigation of the efficiency and effectiveness of the treatment; but they were not informed about the presence of the other group. The variables were measured by tools with psychometric efficiency as described in the following. The variables were evaluated in three stages including before the study (pretest), a week after the end of treatment (posttest), and 12 weeks after the end of interventions (follow up). It should be mentioned that in order to eliminate the probable effects of nuisance variables during the period of follow up, the participants were evaluated every 3 weeks.
Inclusion and exclusion criteria
The inclusion criteria included: the age of 12-18 years, obesity based on BMI≥95th percentile of NCHS/CDC200 standard, no background of receiving pharmacotherapy or psychotherapy over the past 6 months, having no eating disorder except binge eating disorder (based on DSM_5). The exclusion criteria included: 1. the person’s unwillingness to continue participating in sessions, 2. Absence for more than two sessions, 3. Starting a secondary pharmacotherapy or psychotherapy during the research.
Sample size: Regarding the results of similar studies, with the confidence level of 30%, type 2 errors of 25%, and the difference of 2, the sample size was obtained as 18 people in each group. As the follow up period is long, the sample size was considered as 25 people; so that exclusion of the subjects in the case of no bias would not cause any problem in power.

Interventions: Acceptance and commitment therapy (ACT) sessions (30 sessions) (Table 1) and control group individual treatment sessions (1 session a week, twelve 90-min sessions) were held by two clinical psychology masters, one of whom was trained in the area of ACT in treating adolescence disorders (in the experimental group) and the other trained in individual and group counseling in the area of adolescence disorders (psycho-education training in the control group). None of the mentioned psychologists were informed of the type and goal of the research. It should be mentioned that all the subjects of both groups received a therapeutic regimen based on their needs under supervision of a nutrition specialist.
| Therapeutic sessions | Contents |
|---|---|
| First Session | Introducing the basics of treatment :
1. Familiarity with group members and therapeutic relationship, defining rules governing treatment sessions and discussing privacy, clarifying therapeutic relationship, introducing and measuring anxiety and self-esteem, a description of treatment 2. Starting creative helplessness in parents by using metaphor, monster drawing . 3. Investigating parental control strategies, behaviors, and needs using island metaphor. |
| Second Session | Creative helplessness :
1. Receive parental feedback from previous sessions and examine parent island behavior 2. Parents were asked to leave and ask adolescents to come in 3. Open dialogue with teens, expressing values using the metaphor of climbing 4. Creative helplessness, hungry tiger metaphor and pit bull metaphor, homework presentation. |
| Third and Fourth Sessions | Review of previous session assignments, review of creative helplessness, pit metaphor, assessment of organ problems from treatment perspective Talk about the inner world and its difference with the outside world, polygraph metaphor and its relation to emotions |
| Fifth Session | Pre-session assignments are reviewed, introducing control as a problem, highlighting the inefficiency of controlling negative events using metaphors, and training the tendency for negative emotions and experiences. |
| Sixth Session | Introducing Acceptance as an Alternative to Control, Guests Metaphor, learning a non-Judgmental View |
| Seventh Session | Examine assignments and receive feedback from the previous session, familiarity with the hidden features of the language that cause interference, fault expression and bus metaphor, assignment presentation |
| Eighth and Ninth Sessions | Training Mindfulness Techniques and the Relationship of Mindfulness Exercises with Impulsive Behaviors, Emotion, feeling and Thoughts Monitoring Training. |
| Tenth Session | Introducing self-types, chess metaphor, identifying members' life values, and measuring values based on their importance. |
| Eleventh Session | Providing practical solutions to overcoming barriers while employing metaphors and planning for a commitment to pursue values in weight loss. |
| Twelth Session | Summary of concepts reviewed during meetings. Members are asked to share their findings from the Sessions. |
Table 1. The content of ACT treatment sessions.
Risky decision making test (IOWA gambling task): It is a tool used for investigating the person’s decision making in real situations. The participants are faced with 4 cards. In spite of a larger reward, the first two cards can sometimes contain high negative scores; whereas, the last two cards include less rewards and also very lower losses in the case of failure. Table 2 presents the distribution of rewards and scores of this tool. The final score is obtained by deducting the total scores of the first two cards from the total scores of the last two cards. In the present research, this assignment was performed by PC version of this test which has a reliability and validity consistent with the traditional test [29-34].
| Card A | Card B | Card C | Card D | |
|---|---|---|---|---|
| $100 | $100 | $50 | $50 | Win Rate |
| $150-$350 | $1250 | $50 | $250 | Loss Rate |
| 25:25 | 45:5 | 25:25 | 45:5 | The ratio of winning to losing in fifty attempts |
Table 2: The scoring rules in risky decision making test.
Food addiction: This structure was evaluated by Yale food addiction scale. This questionnaire is a 27-item self-assessment tool scored by Likert scale (from never-0 to “4 times or more”-4). It investigates the food addiction severity and assigns people a score of 0-180 [35]. The tool reliability was obtained as 0.94 by Cronbach’s alpha, and checking the validity by confirmatory factor analysis showed a good fitness [36].
BMI: BMI is calculated by measuring height (m) and weight (kg) [36].
Statistical method
Checking demographic data (frequency, mean, and standard deviation) and variance analysis test were done by repeated measures ANOVA in SPSS 16 software.
Ethical considerations
Before the study, a written informed consent letter was received from all the participants. The tools used in this research were all anonymous and an ID code was used for keeping the privacy of the personal information (ethics code: ir.kaums.rec.1395.). Also at the end of the research process, acceptance and commitment therapy was employed in the control group. Furthermore, the research has been registered in Registry of Clinical Trials and the authors do not have any conflict of interests (TCTR20191216003).
Before performing the research, 50 people were randomly selected and randomly assigned to two groups. During the study, in the intervention group, one person left the research due to unwillingness to participate in the study and two people were absent and did not answer the researchers’ calls due to unknown reasons. In the control group, an adolescent was excluded from the study due to the use of cannabis; another person who was absent in follow up was also excluded from study. So, the study was performed on 45 people during 12 weeks of intervention and 12 weeks of follow up. In terms of demographic variables, there was no difference between the two groups regarding their age and their parents’ education (p˂0.01). The data are presented in Table 3.
| Variable | Intervening Group Mean (Standard Deviation) |
Control Group Mean (Standard Deviation) |
Significance Level |
|---|---|---|---|
| Age | 15.22 (1.74) | 15.1(2.22) | 0.086b |
| Mother’s Education Status a | 0.49c | ||
| Middle School Degree | 4 (18)a | 4 (17.39)a | |
| High School Degree | 15(68.19)a | 13 (56.52)a | |
| University Degree | 3(13.7) | 5 (17.85)a | |
| father’s Education Status a | 0.68c | ||
| Middle School Degree | 5 (22.72)a | 4 (17.39) a | |
| High School Degree | 14 (63.63) a | 14 (60.86) a | |
| University Degree | 3 (13.63) a | 5 (21.73) a |
Table 3: The mean and standard deviation of demographic variables in the intervention and control groups.
a. Data presented in N% form
b. Independence T-test was used
c. Chi-square test was used
Table 4 presents the mean scores of risky decision making in three stages of pretest, posttest, and follow up. Regarding the mean scores of pretest, no significant difference was observed between the two studied groups before the intervention (p˂0.05). The results of repeated measures ANOVA for comparison of the changes of decision making scores showed that in posttest and follow up, the mean score of this variable in the experimental group was significantly higher than the control group (p˂0.001) (Table 4). These changes are presented in Table 4 and Figure 1.
| Pre-test | Post-test | Follow-up | Statistical Feature | ||||
|---|---|---|---|---|---|---|---|
| Intervening Group | Control Group | Intervening Group | Control Group | Intervening Group | Control Group | ||
| Risky Decision Making | -6.5(6.06) | -6.34 (4.89) | 1.54(0.08) | -2.17(5. 5) | 4.59 (6.6) | -1.95 (5.26) | p<0.001 F=15.02 |
Table 4: The mean scores of RDM in the experimental and control groups in the three stages.
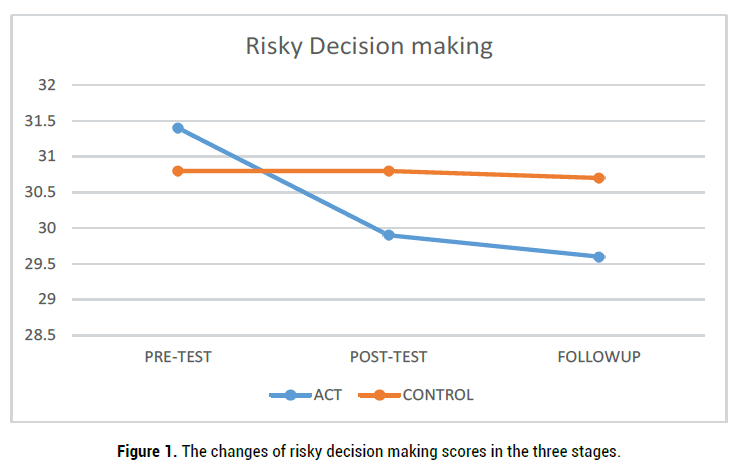
Figure 1. The changes of risky decision making scores in the three stages.
Table 5 presents the mean scores of food addiction severity in the three stages of pretest, posttest, and follow up. Regarding the pretest scores, no significant difference was observed between the two studied groups before the intervention (p˂0.05). The results of repeated measures ANOVA for comparison of the changes of food addiction score showed that in the experimental group, posttest and follow up scores of this variable were significantly higher than the control group (p˂0.001) (Table 5). These changes are presented in Table 5 and Figure 2.
| Pre-test | Post-test | Follow-up | Statistical Feature | ||||
|---|---|---|---|---|---|---|---|
| Intervening Group | Control Group | Intervening Group | Control Group | Intervening Group | Control Group | ||
| Food addiction severity | 31.18(14.85) | 32.86(14.05) | 20.13(20.74) | 29.17(12.6) | 21.86(13.48) | 30.34(10.36) | p<0.001 F=18.025 |
Table 5: The mean scores of food addiction in the experimental and control groups.
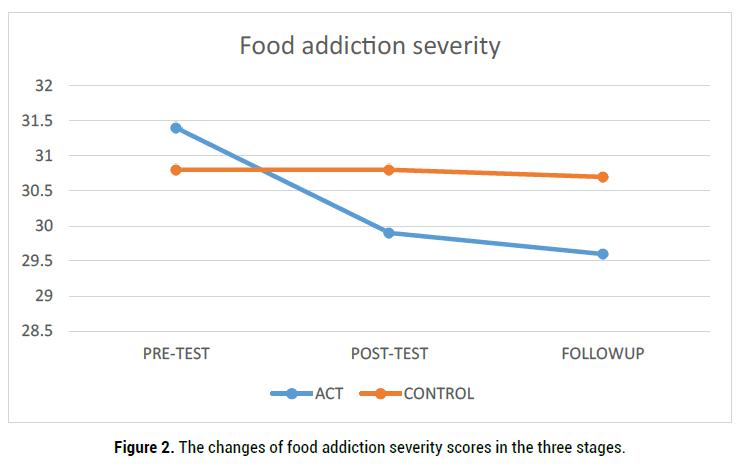
Figure 2. The mean scores of BMI in the experimental and control groups in the three stages.
Table 6 presents the mean scores of BMI in the three stages of pretest, posttest, and follow up. Regarding the mean scores of pretest, no significant difference was observed between the two studied groups before the intervention (p˂0.05). The results of repeated measures ANOVA for comparison of the changes of BMI showed that in posttest and follow up, the mean score of this variable in the experimental group was significantly higher than the control group (p˂0.001) (Table 4). These changes are presented in Table 6 and Figure 3.
| Pre-test | Post-test | Follow-up | Statistical Feature | ||||
|---|---|---|---|---|---|---|---|
| Intervening Group | Control Group | Intervening Group | Control Group | Intervening Group | Control Group | ||
| BMI | 31.04(0.84) | 30.80(0.7) | 29.9(1.5) | 30.8(0.98) | 29.6(1.66) | 30.7(0.96) | P=0.02 F=5.5 |
Table 6: The mean scores of BMI in the experimental and control groups in the three stages
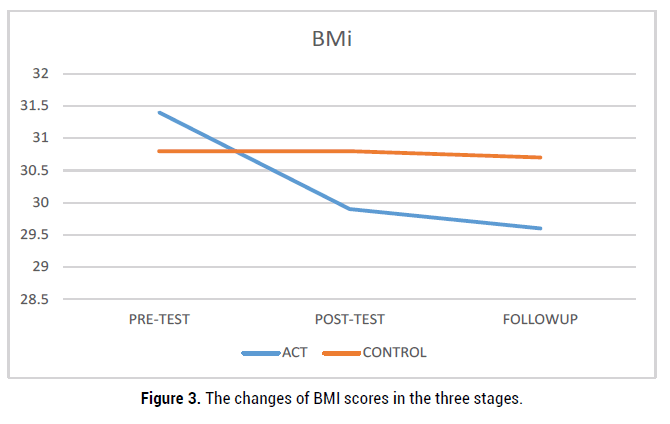
Figure 3. The changes of BMI scores in the three stages.
The present study was performed with 12 weeks of intervention and 12 weeks of follow up, and it showed that integrated acceptance and commitment therapy (ACT) and therapeutic regimen can improve food addiction index, risky decision making, and BMI (weight) in adolescent girls with overweight and obesity.
Although the research literature in this area is so limited, the results of the few studies performed in this field are consistent with the findings of the present research. First, the studies investigating the similar variables to those of this research are reviewed and then, effectiveness of this treatment on the variables (due to consistency) is explained.
The study performed by Nouryan (2015) investigated the effectiveness of acceptance and commitment therapy on women’s obesity. The results suggested that this treatment has significantly decreased BMI in women with overweight and obesity [37].
Lillis (2009) investigated the effectiveness of acceptance and commitment therapy on weight loss. This study was performed with a 12-week follow up (similar to the present study); the results showed that this treatment is significantly effective in weight loss in obese people [38].
The findings of this research and the study performed by Dalen et al (2011) suggested that eating-based mindfulness intervention is significantly effective in improvement of eating behaviors and it can adjust emotional and impulsive eating behaviors. In fact, it leads to improvement of risky decision making in these people [39].
In another study on mindfulness (a fundamental component of acceptance and commitment therapy), it was found that this treatment decreases emotional eating behaviors and emotional addicting behaviors in obese people; this finding is consistent with the results of the present study [40].
Cattivelli et al. explained that acceptance and commitment therapy has a significantly higher research and practical capacity than cognitivebehavioral treatment in treating food addiction [41]. This finding is also consistent with the results of the present research.
In the area of risky decision making, rather than merely focusing on the content and cause of the behaviors, acceptance and commitment therapy is focused on the function of the person’s behavior as a system. By balancing the attention to internal and external stimuli, this approach seeks for improving decision making and moving towards the future sustainable strengthening of the organism. Successfully applying acceptance and commitment therapy leads to a shift from getting involved in impulsive behaviors for instantaneous satisfaction to purposive behaviors adopted by the risky decision making system. The core process of the mentioned shift is flexibility. This process is the negative point of inflexibility and it is specified by behaviors such as paying excessive attention to the future or past, considering the internal experiences as mere truth, extreme dependence on self-related beliefs, and hardly trying to change or deny the internal experiences (such as thoughts and emotions). Acceptance and commitment therapy improves defective emotion regulation in making risky decisions by focusing on increasing flexibility, changing the person’s relations with internal experiences, and specifying the values and beliefs [42-44].
Due to non-judgmental observation, increased awareness and living in the moment, and avoiding refrain, ACT training enables the person to cope with stressful conditions such as addiction; it can be stated that ACT can be effective in decreasing the recurrence, increasing treatment adherence, preservation of the treatment results, and consequently, decreasing addictive behaviors such as food addiction [41]. This treatment employs direct actions and indirect verbal processes for creating more psychological flexibility by acceptance, cognitive defusion, committed action patterns, values, self-as-context, and contacting the present moment. These components encourage the patients to move towards their goals in spite of the obstacles and problems and get rid of negative emotions and thoughts such as frustration, craving, binge eating thoughts, and stress caused by food craving. In this way, in addition to achieving their goals, they can promote their planning and decision making abilities and become successful in weight loss [45]. So, the changeable areas are emphasized and overweight, binge eating, and food addiction (as an emotion-based coping mechanisms) will decrease [41,46].
In spite of the discussed results, this research was faced with some constraints. First, the male gender was not investigated in this study. Second, there was no group to receive the third wave treatments in order to investigate the most effective components of the treatment. It is suggested to investigate the results of similar studies by studying the mediator or intervening variables. Also, it is suggested to investigate other structures affecting food addiction and binge eating behaviors such as emotion regulation and coping mechanisms.
Hereby, we appreciate all the nutrition specialists who helped us in conducting this study. We also sincerely appreciate Rahnamoud Sazan Sepahan Co. For financial support of this research.
Citation: Mohammadreza, Davoudi. Investigation of the Effectiveness of Integrated Acceptance and Commitment Therapy (ACT) and Therapeutic Regime on Food Addiction Severity Index, Risky Decision Making and BMI in Adolescent Girls with Over Weight and Obesity. Clin Exp Psychol, 2021, 7(11), 283.
Received: 05-Oct-2021 Published: 29-Nov-2021
Copyright: © 2021 Davoudi M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.