Research Article - (2021) Volume 10, Issue 10
Background: The mini-tight rope suspensionplasty is a relatively new surgical procedure for treatment of carpometacarpal arthritis. Carpometacarpal arthritis is becoming a frequent diagnosis seen in hand surgery and hand therapy. There is currently minimal research available regarding the post- operative therapy progression and the outcomes related to post-operative management after mini-tight rope suspensionplasty. Therefore, we ask, is a CMC mini-tight rope suspensionplasty, combined with a post-operative therapy course, a favorable option to improve function, increase strength, and decrease pain?
Methods and findings: Twenty six participants underwent the mini-tight rope suspensionplasty procedure and were progressed through the post-operative therapy protocol. Therapy lasted 10 weeks post-operation and measurements were taken pre-operation and at crucial intervals of six weeks, 10 weeks, and six months post-operation. Repeated measures ANOVA indicated significant decrease in QuickDASH scores (3, 9=34.852, p=.000) with a large effect size (partial ETA2=.921), as well as significant decrease in pain rating (3, 10=15.812, p=.000) with a large effect size (partial ETA2=.826). Overall range of motion and grip and pinch strength improved as well.
Conclusions: This surgical procedure and post-operative rehabilitation protocol appears to be a good option for improving function, increasing strength, and decreasing pain in patients with CMC joint arthritis. Furthermore, the rehabilitation protocol appears to expedite the recovery while reducing the common risks of complimentary approaches such as pin tract infection and excessive joint stiffness.
Level of evidence: III
CMC arthritis • Mini-tight rope suspensionplasty • Thumb pain
Study design
This is a level III study, using a one group, pretest-posttest design [1]. From 2010 to 2012, 22.7 percent of the adult population in the United States reported physician-diagnosed arthritis.2 Arthritis prevalence increases with age and is more common in women than men.2 As the population continues to age, the prevalence of arthritis is expected to continue to increase.2 Arthritis is the leading cause of disability among adults in the United States, with about 43 percent of the adult population with arthritis reporting limitations in their daily activities as a result of their arthritis [2,3].
Carpometacarpal (CMC) arthritis is a debilitating, progressive disease which causes decreased function of the thumb and pain with use [4,5]. The CMC joint allows a wide-range of movement in three planes, making the joint prone to degeneration [4-6]. Consistent with the nature of arthritis, CMC arthritis increases with age, and is also predominantly seen in postmenopausal women [7]. A 2007 literature review by Dias et al. showed a strong correlation between excessive basal joint laxity and the development of premature degenerative changes [7]. As ligamentous laxity is common in young women, repeated loading of subluxed joints throughout young adulthood may be the cause for one third of women over 50 showing some radiological evidence of degenerative change.7 However, the most common cause for CMC arthritis is idiopathic [7].
Individuals with CMC arthritis generally present with a gradual, insidious onset of pain localized to the base of the thumb that generally radiates into the thenar eminence and the Metacarpophalangeal (MCP) joint [6,7]. An increase in pain usually correlates to an increase in activity, particularly with forceful pinch and grip or torqueing forces, such as opening a jar, wringing out wash rags, and turning door knobs [7]. Decrease in strength, loss of motion, and decrease in function are also often reported [4,7]. As the degenerative process continues, collapse of the thumb may occur. This produces a swan- neck deformity including adduction of the first metacarpal and compensatory hyperextension of the MCP joint, and radial migration of the base of the first metacarpal, which results in decreased opposition [4,7].
Prehensile ability of the thumb plays a large role in normal hand function [8]. As the thumb provides about 40 percent of hand function, limitations at the CMC joint can have a significant burden on an individual’s well-being [6]. Therefore, CMC arthritis is the most common degenerative condition of the hand in which surgical treatment is sought [5]. An attempt at conservative treatment is often the first option for individuals with CMC arthritis. Conservative treatment can include splinting, injection, anti-inflammatories, strengthening, and activity modification [6,7]. When conservative treatment fails, there are a variety of surgical techniques used to treat CMC arthritis. The goals of any surgical technique are pain relief and improved function [5,7].
A common surgical procedure to treat CMC arthritis, which has been supported by meta-analyses, is a trapeziectomy with the CMC space stabilization supported by a Kirschner wire (K-wire) [9]. Some disadvantages of this surgery include irritation or infection from the K-wire and immobilization for four to five weeks while the K-wire is in place. Recently, a fairly new surgical technique is being utilized which involves a partial or complete trapeziectomy with suture button suspensionplasty utilizing a mini-tight rope between the first and second metacarpals to maintain the CMC joint space [9]. The tightrope provides stability that is comparable to K-wire fixation, however eliminates the chance of irritation or infection from the K-wire. It also allows for early Range Of Motion (ROM) [5,9,10]. Early initiation of rehabilitation can reduce time of recovery, which in turn can improve patient satisfaction and allow for quicker return to work and prior level of daily function [10].
Limited research has been performed regarding outcomes utilizing suture button suspensionplasty. In 2010, Yao et al. performed a study to determine if suture button suspensionplasty maintained post trapeziectomy space height of the first metacarpal by using cadavers [5]. Results indicated that suture button suspensionplasty maintains similar post trapeziectomy space height when compared to K-wire fixation [5].
In 2013, Yao and Song performed a retrospective study in which they reviewed the results of individuals that underwent partial or full trapeziectomy with suture button suspensionplasty at a minimum of two years post operation [11]. The study included 21 patients who were evaluated at least two years after surgery.11 Yao and Song (2013) concluded favorable results in treating CMC arthritis with minimal risks and outcome measures that are similar to previous surgical techniques [11].
In order to further explore the use of mini-tight rope suspensionplasty as treatment for CMC arthritis, there is a need to further determine if the procedure produces favorable results. Therefore we ask, is a CMC mini-tight rope suspensionplasty, combined with a post-operative therapy course, a favorable option to improve function, increase strength, and decrease pain?
The purpose of this study is to substantiate the evidence supporting CMC mini-tight rope suspensionplasty and a post-operative course of rehabilitation as a viable option to improve function, increase strength, and decrease pain in individuals with CMC joint arthritis. The results of this study may provide rehabilitation and medical professionals with information to help identify a viable surgical approach and post-operative rehabilitation course to successfully address CMC joint arthritis.
This is a level III study, using a one group, pretest-posttest design [1]. Approval from the Institutional Review Board (IRB) from the University of Evansville was given before beginning data collection.
Hypotheses
The participants will experience improvements in function and strength as well as a decrease in pain.
Delimitations and limitations
The results of this study apply only to individuals with CMC joint arthritis who have undergone CMC mini-tight rope suspensionplasty. This study is limited to a convenience sample over a period of six months. This study will not apply to populations not included in the subject sample.
Definitions
Thumb spica orthosis: Rigid splint that immobilizes wrist and the thumb. The Interphalangeal (IP) joint of the thumb is left free.
Neoprene thumb spica orthosis: Soft splint providing support to wrist and thumb. This splint allows for ROM, but provides support and limits end ranges of ROM of wrist and thumb.
Subjects
Participants included a convenience sample of patients being treated by one of three hand surgeons at Tri-State Orthopeadic Surgeons for CMC arthritis. Participants were selected over a one year period. Following the decision to undergo mini-tight rope suspensionplasty, a consent form was issued to the patient explaining the research study and any risks involved.
Inclusion criteria included patients who were 30 years of age or older with CMC arthritis and decided to proceed with the mini-tight rope suspensionplasty as a treatment option. Exclusion criteria included any secondary medical condition that could affect healing, low mental capacity, and individuals under the age of 30.
Potential risk of subjects: Testing procedures and treatment techniques are all currently being used as a standard of care in our clinics. There has not been an adverse event to date. All procedures are considered to be safe and non-invasive to the patient. There will be no more than minimal risk to the participants in this study.
Breach of confidentiality of participants’ data is a potential risk and was managed carefully to minimize this risk. An identification number code was used in place of the participants’ name on the study questionnaire. The data was stored in a locked file in the principal investigator’s office. The principal investigator created a file containing the numeric identification code-subject name link for all participants’ data. The file was stored in a separate locked file in the investigator’s office. The information linking each participant’s name and participant code was destroyed after data collection was complete and all data was entered into the study computer. Only the participants’ numeric identification codes appear in the computer.
Setting
Participants included patients of one of two hand surgeons. Participants underwent the mini-tight rope suspensionplasty in an outpatient surgical center and were sent to the outpatient orthopaedic clinic for therapy in southern Indiana.
Procedures
Post-operation therapy protocol: The participants were sent to therapy within three days after surgery. At the initial post-operative visit, the postoperative dressing was removed and a custom fabricated a thumb spica orthosis was fabricated out of Ez Form thermoplastic material. The orthosis allowed the IP joint of the thumb to be free. The participants were instructed to wear this splint full time, removing only for skin care and incision care if needed at home. The participants were advised to avoid all wrist and thumb ROM with the exception of IP ROM. Participants were instructed on tendon gliding techniques and thumb IP ROM in their thumb spica orthosis. IP ROM allowed for active extensor pollicis longus excursion through the area of the surgical incision. Edema gloves, tubigrip, and instruction in the use of ice were provided as needed for edema control.
At 12 to 15 days post operation, sutures were removed and the participants were instructed in scar massage and issued scar molds for nighttime wear over their incision site. Active Range Of Motion (AROM) of the wrist and thumb CMC and MP joints was initiated at this visit. The participants removed the thumb spica orthosis three to four times per day to perform AROM exercises and were allowed to remove the thumb spica orthosis for bathing. The participants continued full time thumb spica orthosis wear between exercises and bathing.
At three weeks post operation, the rigid thumb spica orthosis was discontinued and the participants were issued a neoprene wrist and thumb wrap for full time wear. Again, the participants removed the neoprene wrist and thumb wrap three to four times per day for AROM exercises and were able to remove the neoprene wrist and thumb wrap for bathing. The participants were allowed to use their surgical hand for light activities of daily living, within pain free limits.
At five weeks post operation, the participants were instructed on gentle wrist and grip strengthening exercises, which were performed two to three times per day. The participants were allowed to gradually progress activities with their surgical hand within pain free limits and with a five pound weight restriction. The participants were instructed to wean from the neoprene wrist and thumb wrap as tolerated. At six weeks post operation, the participants were instructed on adding pinch strengthening into their home exercise program two to three times per day along with the wrist and grip strengthening exercises. The participants could gradually progress activities as tolerated within pain free limits.
At ten weeks post operation, the participants were released to unrestricted activities as tolerated.
Data collection: Investigators were trained in the testing protocol and performed all of the tests. Participant identity remained confidential as conventional numbering was used to ensure each participant’s name was not associated with their data.
Outcome measures: Baseline measurements were taken with each patient prior to their surgery. Outcome measurements were taken at six weeks, ten weeks, and six months post-surgery. Outcome measures used included the Quick Disabilities of Arm, Shoulder, and Hand (QuickDASH) for patient-reported assessment of function, the Numeric Pain Rating Scale (NPRS) for patientreported assessment of pain, ROM measurements using a goniometer, and strength measurements of grip and pinch using dynamometers for clinicianassessed measurements.
QuickDASH: The QuickDASH is an 11-question standardized, patientreported outcome measure which measures functional impairment in individuals with musculoskeletal disorders of the upper extremity [12]. Psychometric properties of the QuickDASH demonstrate good reliability and validity [12]. Internal consistency was reported at Cronbach’s alpha of .94 and test-retest reliability has been reported at an ICC at .94 [12]. Convergent construct validity was reported at a range from r=.70 to .80 in the areas of pain, overall problem, function, and work.12 Minimally Clinical Important Difference (MCID) was reported at 14 with a 95 percent Confidence Interval (CI) in patients with a variety of forearm and hand symptoms [13].
NPRS: The NPRS is an 11 point scale that ranges from 0, which equals no pain, to 10, which equals the worst pain imaginable [14]. Patients are asked to rate their pain along the scale from 0 to 10 that correlates to their pain intensity in the last 24 hours [14].The NPRS has good sensitivity and produces data that can be statistically analyzed [14].
The NPRS has demonstrated adequate to excellent test-retest reliability in individuals with chronic pain [15]. As Jensen and McFarland (1993) reported, test-retest reliability increases with the number of ratings taken [15]. The NPRS is reported to have excellent internal consistency when tested in populations of individuals with chronic pain and the healthy population [15,16].Excellent criterion validity has also been reported in the healthy population when the NPRS is compared with four other pain rating scales [16]. Finally, Bijur, Latimer, and Gallagher (2003) reported construct validity demonstrated excellent correlation with the Visual Analogue Scale in the emergency room population [17]. MCID is reported at 15 percent in individuals with chronic musculoskeletal pain, and 35 percent demonstrates a minimal change, 67 percent demonstrates a moderate change, 70 percent demonstrates a significant change, and 94 percent demonstrates a complete change in pain in post-operative patients.
Grip: The Jamar handheld, hydraulic dynamometer was used to measure maximal grip strength. Maximal grip measurements using the Jamar dynamometer has been proven valid and also reliable in individuals with CMC arthritis [18,19]. The average grip strength of three trials was used to determine the subject’s grip strength.
Pinch: The Jamar hydraulic pinch gauge is used to measure various pinch strengths. Pinch strength with use of a hydraulic pinch gauge has been proven reliable and valid [19]. Tip pinch, three jaw pinch, and lateral pinch were measured. An average from three trials of each pinch measurement was taken to determine the subjects pinch strength.
ROM: Thumb abduction, MP flexion, IP flexion, and functional opposition was measured using a finger goniometer. These measures were standardized based on recommendations published by the American Society of Hand Therapists.
A total of 26 participants were included in the study, 11 surgeries were performed on the dominant hand and 15 surgeries were performed on the non- dominant hand. The mean age of participants was 62.115 with participants ranging from 47 to 79 years of age. Descriptive and inferential statistics demonstrated a decrease in pain reported and an overall increase in ROM (with the exception of a small decrease in MP flexion), strength, and function. A repeated measures ANOVA was ran on all ten outcome measures reported in order to decrease type 1 error. All ten outcome measures demonstrated significant differences over time and no significant differences between dominant vs. non-dominant hands.
QuickDASH: Pre-op measurements indicated a mean QuickDASH score of 52.5% reported disability. This score decreased gradually over the next 6 months, with a mean measurement of 9.692% reported disability at the 6-month measurement. (Table 1 and Figure 1). Repeated measures ANOVA using Wilks’ Lambda indicated significant decrease in QuickDASH scores (3, 9=34.852, p=.000) with a large effect size (partial ETA2=.921). No significant difference was seen between dominant vs. non-dominant hands (p=.891).
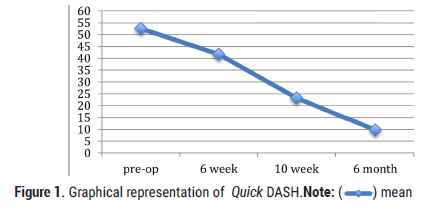
Figure 1: Graphical representation of Quick DASH.Note: ( ) mean
) mean
|
Pre-op | 6 week | 10 week | 6 month |
|---|---|---|---|---|
Mean |
52.5 | 41.667 | 23.235 | 9.692 |
Median |
51 | 41 | 18 | 7 |
Range |
80 | 77 | 66 | 43 |
Table 1. Pre-op measurements of QuickDASH.
NPRS: Pre-op measurements indicated a mean NPRS score of 5.65 reported pain. This score decreased gradually over the next 6 months, with a mean measurement of 0.385 reported pain at the 6-month measurement. (Table 2 and Figure 2). Repeated measures ANOVA using Wilks’ Lambda indicated significant decrease in NPRS scores (3, 10=15.812, p=.000) with a large effect size (partial ETA2=.826). No significant difference was seen between dominant vs. non-dominant hands (p=.775).
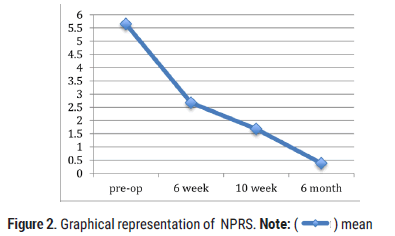
Figure 2: Graphical representation of NPRS. Note: ( ) mean
) mean
| Pre-op | 6 week | 10 week | 6 month | |
|---|---|---|---|---|
| Mean | 5.65 | 2.667 | 1.684 | 0.385 |
| Median | 6 | 3 | 1 | 0 |
| Range | 9 | 9 | 5 | 2 |
Table 2. Pre-op measurements of NPRS.
ROM: Pre-op measurements indicated a mean MP flexion of 46.885 degrees. This measurement decreased over the next 6 months, with mean a measurement of 43.846 degrees at the 6-month measurement. (Table 3 and Figure 3). Repeated measures ANOVA using Wilks’ Lambda indicated significant decrease in MP flexion measurement (3, 10=4.722, p=.026) with a large effect size (partial ETA2=.587). No significant difference was seen between dominant vs. non-dominant hands (p=.055).
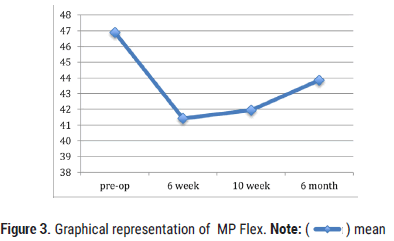
Figure 3. Graphical representation of MP Flex. Note: ( ) mean
) mean
| Pre-op | 6 week | 10 week | 6 month | |
|---|---|---|---|---|
| Mean | 46.885 | 41.429 | 41.947 | 43.846 |
| Median | 49.5 | 42 | 40 | 42 |
| Range | 59 | 39 | 30 | 30 |
Table 3. Pre-op measurements of MP Flex.
Pre-op measurements indicated a mean IP flexion of 44.46 degrees. This measurement increased over the next 6 months, with mean a measurement of 63.231 degrees at the 6 month measurement. (Table 4 and Figure 4). Repeated measures ANOVA using Wilks’ Lambda indicated significant increase in IP flexion measurement (3, 10=6.12, p=.012) with a large effect size (partial ETA2=.647). No significant difference was seen between dominant vs. non- dominant hands (p=.099).
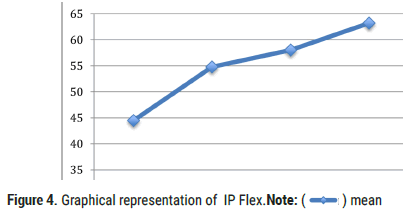
Figure 4. Graphical representation of IP Flex. Note: ( ) mean
) mean
| Pre-op | 6 week | 10 week | 6 month | |
|---|---|---|---|---|
| Mean | 44.46 | 54.762 | 58.053 | 63.231 |
| Median | 46.5 | 55 | 63 | 62 |
| Range | 72 | 43 | 36 | 36 |
Table 4. Pre-op measurements of IP Flex.
Pre-op measurements indicated a mean abduction of 40.231 degrees. This measurement increased over the next 6 months, with a mean measurement of 60.769 degrees at the 6 month measurement. (Table 5 and Figure 5). Repeated measures ANOVA using Wilks’ Lambda indicated significant increase in abduction measurement (3, 10=3.936, p=.043) with a large effect size (partial ETA2=.541). No significant difference was seen between dominant vs. nondominant hands (p=.341).
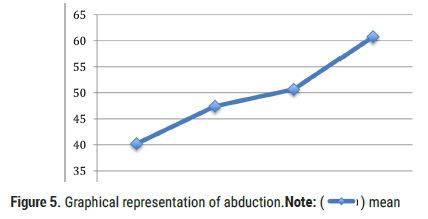
Figure 5. Graphical representation of abduction.Note: ( ) mean
) mean
| Pre-op | 6 week | 10 week | 6 month | |
|---|---|---|---|---|
| Mean | 40.231 | 47.429 | 50.684 | 60.769 |
| Median | 40 | 45 | 48 | 60 |
| Range | 71 | 52 | 44 | 50 |
Table 5. Pre-op measurements of abduction.
Pre-op measurements indicated a mean opposition of 4.858 centimeters. This measurement increased over the next 6 months, with mean a measurement of 6.492 centimeters at the 6 month measurement. (Table 6 and Figure 6). Repeated measures ANOVA using Wilks’ Lambda indicated significant increase in opposition measurement (3, 10=5.475, p=.017) with a large effect size (partial ETA2=.622). No significant difference was seen between dominant vs. non-dominant hands (p=.971).
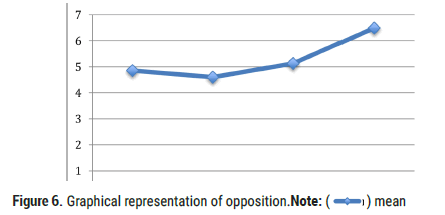
Figure 6. Graphical representation of opposition.Note: ( ) mean
) mean
| Pre-op | 6 week | 10 week | 6 month | |
|---|---|---|---|---|
| Mean | 4.858 | 4.6 | 5.126 | 6.492 |
| Median | 5.1 | 5.5 | 5.6 | 6.5 |
| Range | 9.5 | 9 | 7 | 4.3 |
Table 6. Pre-op measurements of opposition.
Strength: Pre-op measurements indicated a mean grip strength of 39.3 pounds. This measurement increased over the next 6 months, with a mean grip strength of 55.6 pounds at the 6 month measurement. (Table 7 and Figure 7). Repeated measures ANOVA using Wilks’ Lambda indicated significant increase in grip strength (3, 10=18.523, p=.000) with a large effect size (partial ETA2=.847). No significant difference was seen between dominant vs. nondominant hands (p=.632).
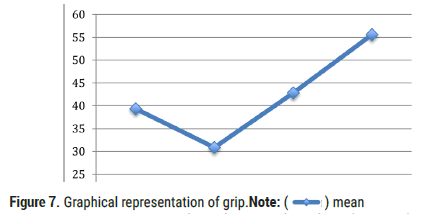
Figure 7. Graphical representation of grip. Note: ( ) mean
) mean
| Pre-op | 6 week | 10 week | 6 month | |
|---|---|---|---|---|
| Mean | 39.3 | 30.851 | 42.825 | 55.6 |
| Median | 34 | 27.3 | 38 | 49 |
| Range | 81.3 | 94 | 66.3 | 70.3 |
Table 7. Pre-op measurements of grip.
Pre-op measurements indicated a mean lateral pinch strength of 7.395 pounds. This measurement increased over the next 6 months, with a mean lateral pinch strength of 10.223 pounds at the 6 month measurement. (Table 8 and Figure 8). Repeated measures ANOVA using Wilks’ Lambda indicated significant increase in lateral pinch strength (3, 10=5.199, p=.020) with a large effect size (partial ETA2=.609). No significant difference was seen between dominant vs. non-dominant hands (p=.054).
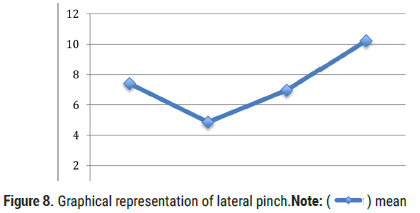
Figure 8. Graphical representation of lateral pinch.Note: ( ) mean
) mean
| Pre-op | 6 week | 10 week | 6 month | |
|---|---|---|---|---|
| Mean | 7.395 | 4.856 | 6.963 | 10.223 |
| Median | 7.5 | 4 | 7 | 9 |
| Range | 16.7 | 15.7 | 8.8 | 10.3 |
Table 8. Pre-op measurements of lateral pinch.
Pre-op measurements indicated a mean tip pinch strength of 4.796 pounds. This measurement increased over the next 6 months, with a mean lateral pinch strength of 7.982 pounds at the 6 month measurement. (Table 9 and Figure 9). Repeated measures ANOVA using Wilks’ Lambda indicated significant increase in tip pinch strength (3, 10=7.888, p=.005) with a large effect size (partial ETA2=.703). No significant difference was seen between dominant vs. non-dominant hands (p=.439).
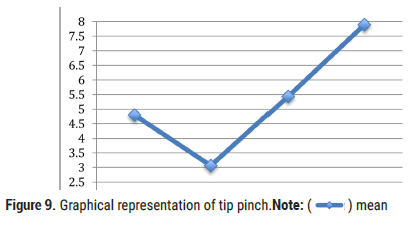
Figure 9. Graphical representation of tip pinch.Note: ( ) mean
) mean
| Pre-op | 6 week | 10 week | 6 month | |
|---|---|---|---|---|
| Mean | 4.796 | 3.062 | 5.435 | 7.982 |
| Median | 4.7 | 2 | 5 | 7 |
| Range | 12.7 | 9 | 11.8 | 13.4 |
Table 9. Pre-op measurements of tip pinch.
Pre-op measurements indicated a mean 3-jaw pinch strength of 6.085 pounds. This measurement increased over the next 6 months, with a mean 3-jaw pinch strength of 9.385 pounds at the 6 month measurement. (Table 10 and Figure 10). Repeated measures ANOVA using Wilks’ Lambda indicated significant increase in 3-jaw pinch strength (3, 10=23.170, p=.000) with a large effect size (partial ETA2=.874). No significant difference was seen between dominant vs. non-dominant hands (p=.214).
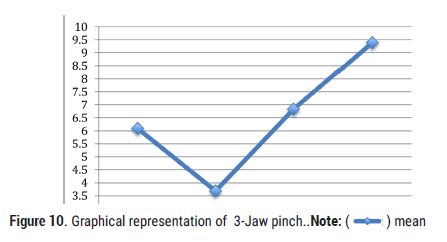
Figure 10. Graphical representation of 3-Jaw pinch. Note: ( ) mean
) mean
| Pre-op | 6 week | 10 week | 6 month | |
|---|---|---|---|---|
| Mean | 6.085 | 3.681 | 6.829 | 9.385 |
| Median | 6.5 | 3 | 6.3 | 8 |
| Range | 15 | 10 | 10.3 | 12.7 |
Table 10. Pre-op measurements of 3-Jaw pinch.
All areas of measurement demonstrated statistically significant change. QuickDASH scores and NPRS rating indicated the most clinically significant progress throughout this study. Interpreted, this demonstrates that participants demonstrated a significant increase in perceived daily function as well as a significant decrease in perceived pain. These two factors are often the main reasons individuals seek medical attention and proceed with surgical intervention.
MP flexion demonstrated a statistically significant decrease in ROM. However, these authors feel that a decrease in three degrees is not clinically significant and could be related to measurement error. Even without the possibility of measurement error, the researchers feel that this very small decrease in MP flexion did not hinder any participants in any form or fashion based on the significant increase in function and decrease in pain that was demonstrated by significant change in QuickDASH and NPRS ratings. When compared, MP flexion measurements also showed a higher p value and smaller effect size compared to QuickDASH and NPRS ratings.
The mini-tight rope suspensionplasty in combination with the given postoperative therapy protocol appeared to demonstrate favorable results. This surgical procedure, along with the post-operative rehabilitation appear to decrease pain and improve function all while expediting the post-operative rehabilitative process. By eliminating infection risks from a pin and allowing early movement, individuals undergoing a mini-tight rope suspensionplasty are able to return to their daily lives, independently, and with less pain in a fairly quick time frame. In addition, statistical evidence supports substantial improvements in abduction, opposition, grip strength, tip pinch strength, lateral pinch strength, and 3 Jaw pinch strength all which contribute to the exceptional gains in functional use of the involved hand. Limitations for this study include the small sample size. Future recommendations for further studies include repeating the study with a greater sample size. Future studies could also look at determining if age and/or activity level play a role in improvements. In addition, future studies may compare these results with results of complimentary surgical approaches of CMC joint arthritis. Overall, the mini-tight rope suspensionplasty and post-operative plan of care can significantly improve an individual’s daily function while decreasing their pain. As our population is aging, the future is a little brighter for individuals suffering from CMC arthritis.
The authors are incredibly appreciative to all the therapy staff at Tri State orthopaedic surgeons for their invaluable assistance throughout the data collection process. The authors would also like to acknowledge Dustin Williams for his assistance with data analysis and Hannah Logsdon for her assistance in data entry.
Citation: Thacker J. “Is a CMC Mini-Tight Rope Suspensionplasty, Combined with a Post-operative Therapy Course, a Favorable Option to Improve Function, Increase Strength, and Decrease Pain?”. J Arthritis, 2021, 10(10), 001-005.
Received: 27-Oct-2021 Published: 17-Nov-2021
Copyright: © 2021 Thacker J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.