Review Article - (2022) Volume 13, Issue 12
Incarcerated people represent a very marginalized population within the United States.The purpose of this review article is to examine common and uncommon neurological conditions that may present within the population of incarcerated and detained adults and juveniles. In this review, we investigate neurological complaints within the realms of learning and intellectual disabilities, epilepsy, sleep disorders, neuroinfectious diseases, nutritional deficiencies, injuries.
Incarcerated people represent a marginalized, underserved patient population in the United States [1, 2]. Within the United States, there are over 2 million people who are incarcerated [3]. Of these people, over 800,000 are incarcerated and in need of care for one or more chronic medical conditions [4].
In prisons, jails and immigration detention, neurological complaints are common, accounting for around 10% of outpatient chief complaints [5]. Incarcerated juveniles and adults require care for numerous neurological conditions, including epilepsy, neuroimmunological disorders, traumatic brain injuries and sequelae of nutritional insufficiencies.
Learning and intellectual disabilities
Within the incarcerated population, there is a higher prevalence of intellectual learning disabilities as compared with the general population. For instance, prevalence of reading and spelling difficulties in prisoners may reach up to 50% while the prevalence of dyslexia in the general population may be closer to 5% [6, 7]. Oral language impairment has been recorded as up to 50% in young offenders [8]. For Attention Deficit Hyperactivity Disorder (ADHD), it is estimated that the prevalence is 5 times higher in juvenile prison populations and 10 times higher in adult prison populations, as compared with the general population [9]. Within police custody, the rate of learning disability may be as high as 10% [10]. Oral language impairments specifically have been found to be correlated with more severe offenses [8]. With Intellectual Disabilities (ID), there is evidence for higher rates of ID within he incarcerated population, 3.77% to 10.8%,while the prevalence of ID among the general population is around 1% [11-13]. For borderline ID, the prevalence may be as high as 7.54% to 11% [14]. One study of 143 prison inmates found a mean IQ of 91.5 [11,12].
Developmental disabilities may have a higher prevalence in the prison population as well. In one study in Ontario, Canada, which defined developmental disability as “significant limitations, including cognitive functioning and adaptive functioning, before the age of 18,” the prevalence of developmental disabilities was 2.2% in the prison group, as compared with 0.7% in the general provincial population of Ontario [15].
Prisoners with intellectual disability may experience other negative health outcomes as well. One study across 7 prisons in Australia found that prisoners with ID had higher rates of heart disease, obesity and hearing problems, and fewer preventative care interventions and immunizations [16]. Even after release, prisoners with developmental disabilities have more emergency department visits and hospitalizations in prison than the general population [15].
Education levels, and potential access to therapies within the school system, amongst the prison population may affect the prevalence of learning disabilities in this population. For example, the majority of the population in Finland completes primary education, whereas only 59% of studied prisoners in Finland had completed primary school [17]. Lower rates of school completion, and resultant smaller exposure to the potential therapies that may be offered in the school setting, may be one factor in the higher rates of learning disabilities seen in the prison population.
Learning and intellectual disabilities may have a profound impact on an individual’s ability to participate in police interviews. Exoneration by DNA evidence allows us to examine how lengthy interrogations, presentation of false evidence, and use of psychological manipulation may precipitate false confessions from innocent people. Intellectual disability may increase the risk of false confessions in an interrogation setting [18-20].
Epilepsy
Epilepsy has up to 3 times or 4 times greater incidence in jail and prison populations than in the general population. Of these patients, within the incarcerated setting, over 70% may have uncontrolled seizures higher than the 33% of epilepsy patients with uncontrolled seizures that would be expected in the general population [21-23].
Uncontrolled epilepsy may be an underlying risk factor for Sudden Unexplained Death In Epilepsy Patients (SUDEP), as are inadequate antiepileptic drug treatment and prone position at time of death [24]. While the exact rate of SUDEP deaths in incarcerated populations is unclear, these factors may be risk factors for epilepsy patients who are incarcerated.
For example, in one case from a patient in a prison in Brixton, England in 1984, a 38 year old man with epilepsy was put to bed after having a generalized seizure, and he was subsequently found dead during a routine check a few hours later [25]. On postmortem examination, his plasma level of phenytoin was 5 mg/L, which is subtherapeutic [26]. On further investigation, it was found that this individual with epilepsy was not given 12 doses out of 18 prescribed doses of his phenytoin in the last week of his life. Hence, while it is possible that he may have had uncontrolled epilepsy even while on a therapeutic regimen seizure medication, the lack of administration of one third of his medication doses likely contributed to his subtherapeutic drug level, breakthrough seizure and subsequent death.
Sleep disorders
Sleep disorders, and overall difficulties with obtaining adequate sleep, are a common problem within detention facilities and prisons [27-29]. While predisposing factors for insomnia may include health status and pre-existing psychiatric issues the circumstances of incarceration itself may predispose people to have difficulty with falling and staying asleep [30, 31].
Complaints of noise, excessive lights, and uncomfortable bedding, or even lack of bedding, all contributed to difficulties with sleep for detained people [32]. Other circumstances in prisons, such as beds being co-opted as living places to eat and watch television, also disrupt sleep hygiene [33].
In detained juveniles, inadequate environments for sleep are common and may result in significant medical and psychiatric sequelae. Within immigrant child detention, there are reports of lack of beds entirely, freezing cold conditions and lights kept on throughout the night [34]. The resulting sleep deprivation from these austere conditions may result in increased rates of depression, neurobehavioral problems, aggression, and type 2 diabetes [35-37,33].
In adults, lack of quality sleep may be associated with increased rates of aggressive behaviors and an international standard of giving incarcerated people at least 6 hours of sleep per night has been proposed [38, 39]. Sleep apnea in particular may be an under-evaluated problem in incarcerated people and this population may benefit from increased dedicated resources for the diagnosis and management of sleep apnea [40, 41]. Rarer conditions, such as narcolepsy, have been seen in incarcerated people and there are difficulties in making diagnoses of less prevalent conditions within the resource-limited prison setting [42].
Neuro-infectious diseases
Infectious diseases with neurological sequelae are a unique set of conditions in the incarcerated population, as distancing measures to decrease transmission of communicable diseases are difficult to implement in facilities. For example, in a study of both incarcerated and non-incarcerated people with Acquired Immunodeficiency Syndrome (AIDS), it was found that complications arising from opportunistic Central Nervous System (CNS) bacterial infections from Mycobacterium tuberculosis (TB) were more common in the incarcerated population than the general population [43].
More recently, the spread of coronavirus disease 2019 (COVID-19) within correctional facilities and immigrant detention has resulted in significant morbidity and mortality , inclusive of neurological complications. The prevalence of COVID-19 within incarcerated populations is more than five times higher than that of non-incarcerated Americans [44, 45]. In particular, prison crowding has been found to increase rates of COVID-19 [46]. To this end, there have been efforts by various states and organization to release non-violent offenders and pre-trial detainees to mitigate the spread of COVID-19 [47].
COVID-19 has been notable for its association with neurological sequelae, including strokes, new-onset seizures, cerebral venous sinus thrombosis, meningoencephalitis, Guillain-Barre syndrome, and olfactory changes [48]. Early in the COVID-19 pandemic, the known early signs of anosmia in the course of COVID-19 infection were used as a screening technique in some prison facilities; in one study, 10 out of 10 screened prisoners who had anosmia were found to be positive for COVID-19 on nasopharyngeal swab [49].
Nutritional deficiencies
In addition to organic diseases of the brain and spinal cord which may present in the incarcerated population, the direct effects of incarceration on nutritional status may cause neurological sequelae. Undernutrition is a prevalent problem in incarcerated individuals, both internationally and in the US. For instance, in one study in Southern Ethiopia in 2020, 23.2% of incarcerated adults were found to be underweight [50].
Within the US, investigation of nutrition provided in county jail has shown evidence of inadequate daily intake of micronutrients, such as vitamin D, magnesium and omega-3 fatty acids Furthermore, even amongst inmates who are provided adequate nutrition through the provided meals, hunger strikes are a common mechanism for inadequate nutrition among incarcerated people [51, 52]. Resulting thiamine deficiency has been linked to peripheral neuropathy amongst incarcerated people [53].
Even in the community, for people who are not currently incarcerated, history incarceration may predispose adults to being undernourished. History of previous incarceration, as well as the duration of imprisonment, are factors that are correlated with undernutrition [54].
Nutritional deficiencies themselves may contribute to violent behavior. In one study of 26 incarcerated juveniles in California with vitamin deficiencies, including those of vitamin B2 (Riboflavin), vitamin B12 (Cobalamin) and folate, these children were randomized to receive either vitamin repletion or placebo. The group that received vitamin supplementation and resultant post-treatment vitamin blood levels within normal limits, these individuals had fewer violent encounters than the individuals in the placebo group [55]. A similar finding of reduction in violent offenses in prisoners who received vitamin supplementation has been found in the adult population as well [56].
In addition to vitamin deficiencies having an effect on violent behavior, vitamin deficiencies may present with more unusual neurological findings.
In one case report of a 24 year old woman who was incarcerated for 4 months in China, she presented with slowed cognition, weakness, dysarthria and amnesia [30-31]. On examination, she had noted horizontal and vertical nystagmus, and nerve conduction studies showed evidence of a sensorimotor axonal polyneuropathy. She was found to have a low thiamine level, in the context of malnutrition from a hunger strike, and subsequent evidence of Wernicke’s encephalopathy on MR imaging (Figure 1). Following IV thiamine repletion, this young woman fully recovered over the next 4 months.
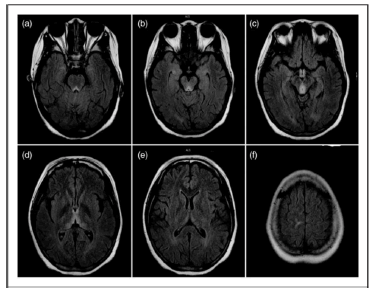
Figure 1: Axial FLAIR images showing hyperintensities of the periacqueductal gray area (a,b) mamillary body, (c) thalamus, (d) frontal ventricle, encephalopathy.
Toxicology
Both during incarceration and upon release, overdoses of both prescription and illicit substances may cause neurological changes [57-59]. In one study of 130 incarcerated adults in Ohio, there were a total of 107 overdoses (100 intentional and 7 unintentional), with phenytoin as the most commonly overdosed drug (22% of cases) [60]. Interestingly, co-morbid ADHD that is adequately treated with prescription stimulants may decrease rates of illegal substance abuse among incarcerated adults [61].
Following release from incarceration, adults are at a high risk of overdose, as early as 2 weeks following release and with increased risk up to 1 year after release from prison [62, 63]. The risk of overdose deaths have been shown to be higher in adults who have been incarcerated within the past 2 years to 5 years [64, 65]. Among those who have been incarcerated, a previous history of serious mental illness, as well as white, nonHispanic race, were risk factors for fatal opioid overdose [66].
To help prevent opioid-related fatalities in people recently released from prison, both naloxone kits and naloxone prescription with education given upon release have shown promise in decreasing mortality rates [67, 68].
Traumatic brain injury
There may be higher rates of Traumatic Brain Injury (TBI) amongst incarcerated people compared to the general population. In one meta analysis of over 5000 incarcerated adults, there was a prevalence of TBI of approximately 51% among the incarcerated group, compared with an estimated prevalence of TBI of 38% in the general population [69]. Similarly, another review of 33 articles, including over 9000 people, found an average prevalence of TBI in prison populations to be around 46% [70].
In another study of 69 randomly-selected inmates within a county jail population, there was a prevalence of 87% of lifetime TBI, and 36% with TBI sustained over the preceding year [71]. In one study of female inmates in the United Kingdom, there was a prevalence of 79% of lifetime TBI, with 38% having a history of 6 or more injuries [72].
There are instances of traumatic brain injuries occurring within correctional facilities. In one case report, a 17-year-old incarcerated young man was involved in an “initiation ceremony” within his cell, which involved multiple blows to the head from his cellmates. Initially, he was conscious, then went to bed, and was found with emesis by his mouth the next day. No head imaging was performed. About 6 weeks later, he was found to have altered mental status, with a documented Glascow Coma Scale of 5, and upon admission to the hospital, had a head CT performed which showed a subdural hematoma with maximum depth of 5 mm. He subsequently died from his injuries, and on autopsy, a clear infarct of the caudate was found, with extension into the thalamus and putamen [73].
There are a number of neurological conditions which may present at higher prevalences within the population of incarcerated people, and some may go unrecognized in this highly vulnerable population in the US. There is limited data regarding many of these conditions and the exact management plans that are available to incarcerated people both within the US and around the world, and more research into this underserved population is needed.
[Crossref]
Citation: Han, S., Nath, A. Neurological Conditions among the Incarcerated: A Medically Underserved Population. J Neuro Neurophysiol. 2022, 13 (12), 001-004
Received: 13-Dec-2022, Manuscript No. jnn-22-83197; Editor assigned: 15-Dec-2022, Pre QC No. jnn-22-83197 (PQ); Reviewed: 19-Dec-2022, QC No. jnn-22-83197 (Q); Revised: 20-Dec-2022, Manuscript No. jnn-22-83197 (R); Published: 30-Dec-2022, DOI: 10.35248/2332- 2594.22.13(12).771
Copyright: ©2022 Han, S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.