Case Study - (2021) Volume 0, Issue 0
Introduction: Esthesioneuroblastoma is a rare malignant tumor, which develops from olfactory neuroepithelium and is one of the rarest tumors of the nasal cavity. Its diagnosis is based on imaging and confirmed by anatom opathology.
Objective: The objective of this study is to analyze through a review of the literature, histoclinical characteristics, therapeutic means and prognostic factors of this tumor.
Study: A retrospective study concerning 6 cases of olfactory neuroblastoma treated at the department of radiotherapy of the University hospital Center in Fez, Morocco, from January 2012 to December 2017.
Results: The average age of our patients was 40 years. Clinical symptomatology was dominated by nasal obstruction and epistaxis. 5 patients were classified as Kadish C and one patient as Kadish D. 4 patients underwent surgical treatment. Concering adjuvant radiotherapy, 2 received a dose of 70 Gy (2 using the three-dimensional conformal radiotherapy technique: 3D), 1 patient received a dose of 66 Gy in 3D, and 1 patient received 66 Gy using conformal radiotherapy with intensity modulation: IMRT. 1 patient had an important loco regional extension and was above any curative treatment, two patients were in complete remission, one patient had progressive continuation, one patient had local recurrence, and the patient who received no treatment was referred to the family.
Conclusion: Olfactory esthesioneuroblastoma is a rare Sino nasal malignant tumor, characterized by clinical polymorphism and local invasion. In spite of the surgery and the radiotherapy, the forecast remains reserved on the long term.
Neuroblastoma • Radiotherapy • Polymorphism • Malignant tumor
Esthesioneuroblastoma (ENB), also known as olfactory neuroblastoma, is an uncommon malignancy of the head and neck, representing only 3% to 6% of nasal cavity and sino nasal neoplasms [1]. First described by Berger, Luc, and Richard [2], ENB is a tumor of neural crest origin that is considered to arise from the olfactory neuroe- pithelium of the olfactory cleft in the superior nasal cavity at the anterior skull base [3]. Local spread of tumor can extend throughout the paranasal sinuses and skull base with invasion of the orbit, cavernous sinus, and brain.
Several treatment approaches for ENB have been described in the literature, but rigorous, prospective treatment studies are absent given the tumor’s rarity and pattern of recurrence that requires an extended posttraitement observation period. The behavior of the tumor varies from an indolent slow-growing neoplasm to that of a highly aggressive and locally invasive malignancy with a capacity for regional and distant metastases. Unfortunately, ENB is typically diagnosed after extensive local spread. However, the advances in surgical and radiation techniques and the use of novel chemotherapeutic approaches have lead to the development of an evolving array of encouraging treatment options reported on this diagnosis [4].
We propose through this study and literature review precising the histo clinical characteristics, as well as the different anatomo clinical classifications of the olfactory esthesio neuroblastomas exploring the elements of prognosis, as well as drawing an adopted therapeutic protocol to this tumor.
The present study is retrospective and descriptive carried out during a 5 year period (2012 to 2017) and based on six observations about olfactory esthesioneuroblastomas compile at the Radiotherapy department of the Hassan II University Hospital (CHU Hassan II) of Fez.
Our series of study included three men and three women, with an age ranging from 21 to 64 ans an average age of 40, and no particular exposing to risk factors were noted. The average time taken by the patient oconsult was 6 months and ranging from 2 months to 1 years, the reason for consultations were mainly the ocular and rhino sinus signs. Imparticular, a unilateral and nasal obstruction was present in 5 cases, an epistaxis of low abondance resistant to treatment was noted in 4 cases, also, some nasal sinus pains were witnessed in 3 cases. Ocular signs were noted in 4 cases and took the form of exophtalmos for 2 patients, and a low visual acquity for three patients. Some neurological signs consisted of headaches, were noted in one case; the physical examination, using the nasal endoscopy performed for 5 of our patients, showed a circonferential process of the nasal cavity in 4 cases. A total filling of the nasal cavity was witnessed in 3 cases and a deviation of the nasal septum to controlateral side in 1 case.
The fundoscopic examination, performed for all our patients, showed signs of vascular damage in 1 case. Besides, the neurological examination indicated a trismus in an other case. The examination of lymph nodes showed some palpable cervical lymphadenopathies for 1 patient. A facial CT scan was carried out for our 6 patients and showed a Kadish stage C tumor of nasal sinus cavities in 5 cases and a Kadish stage D in 1 case. An expansion to the orbital cavités in 2 cases and to the base of the scull in 1 case. Facial MRI was perfomed for 3 patients, and the tumor bondaries were extended more than what CT scan showed before.
The diagnosis of olfactory esthesioneuroblastoma was only retained on the basis of the anatomopathological examination of the biopsies. On the microscopique level, the two predominat criteria were a lober and compact shape (Figure 1-4). The tumor cells were small with rounded nucleolis. Cytoplasm was less abondant, without nuclear membrane and with a proeminent fibrillated matrix. According to the histologic grading of Hyams three cases were stage I, two others were stage II and one case was stage III. An extended assenssment included a thoraco abdominal CT scan done for 4 patients and also a chest X-Ray for two patients, an abdominal sonography for the two other cases, some lymphadenopathies were found in two patients.
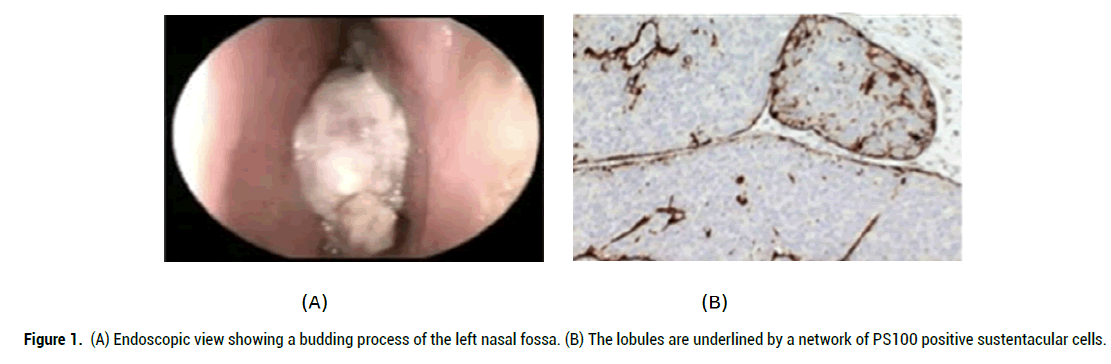
Figure 1: A) Endoscopic view showing a budding process of the left nasal fossa. (B) The lobules are underlined by a network of PS100 positive sustentacular cells.
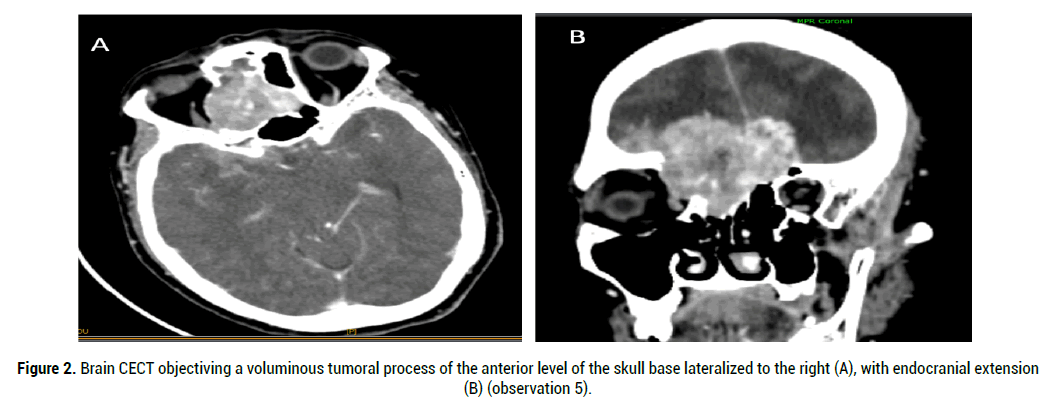
Figure 2: Brain CECT objectiving a voluminous tumoral process of the anterior level of the skull base lateralized to the right (A), with endocranial extension (B) (observation 5).
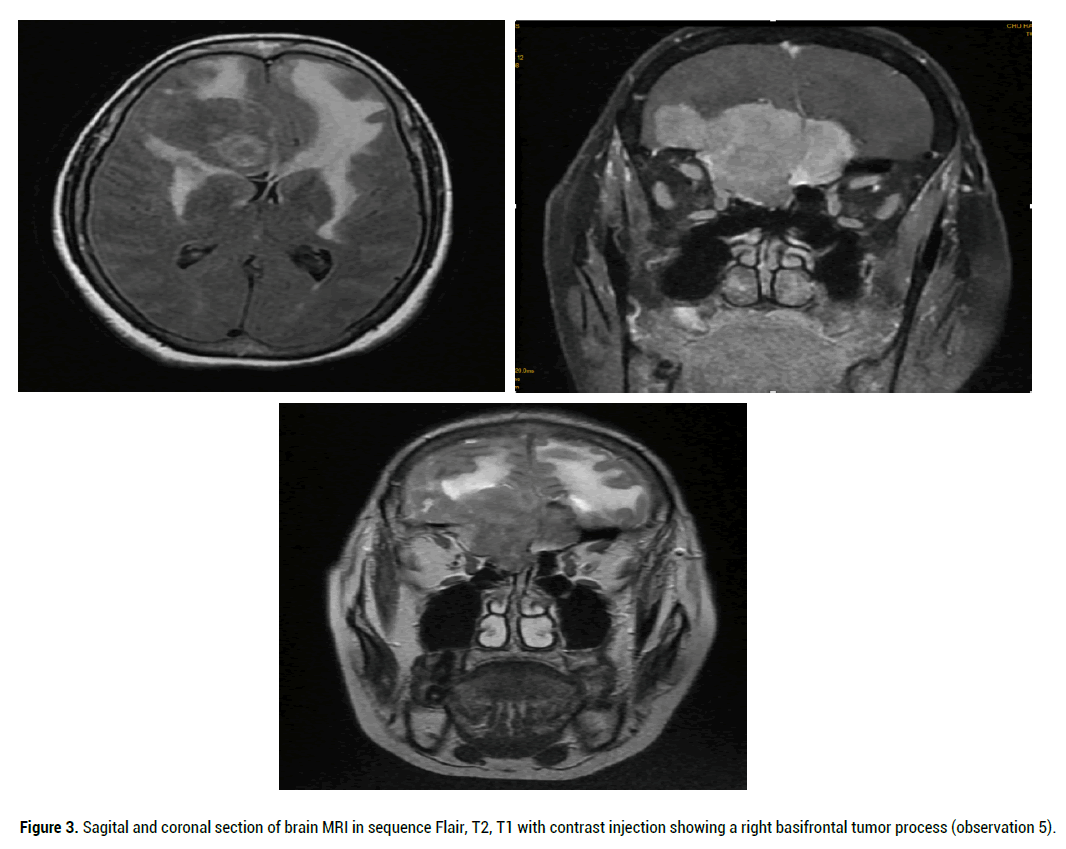
Figure 3: Sagital and coronal section of brain MRI in sequence Flair, T2, T1 with contrast injection showing a right basifrontal tumor process (observation 5).

Figure 4: Brain CECT objectiving a voluminous locally advanced left naso-ethmoido-maxillofrontal tumor process (observation 2).
Four patients had surgeries from which four by the intransal approach, and the 4th by open surgery with extended lymph node dissection. A patient was judged for above any treatment due to the important locoregional expansion of the tumor, then she had a symptomatic treatment (Observation N° 2). The surgical treatment was followed by radiation therapy for 4 patients, 2 received a dose of 70 Gy (using the three-dimensional conformal radiotherapy technique: 3D) and 1 patient received a dose of 66 Gy in 3D, and 1 using conformal radiotherapy with intensity modulation: IMRT (Figures 5-6). One patient had palliative chemotherapy. A complete remission was achived for two patients after 3 years follow up (Table 1).
| Case | Age | Sex | Time of consultation | Clinical symptoms | Staging | Traitement | Evolution |
|---|---|---|---|---|---|---|---|
| 1 | 25 | M | 12 months | Nasal Obstruction. Exophtalmos. low visual acquity Headaches. |
Stage C | Surgery radiation therapy |
Full remission |
| 2 | 30 | M | 8 months | Epistaxis, Nasal sinus pains Swelling of the hemiface |
Stage D | Symptomatic traitement | Patient deliverad to family |
| 3 | 21 | M | 2 months | Nasal Obstruction. Epistaxis, anosmia -Low visual acquity Nasal sinus pains -Headaches |
Stage C | Surgery radiation therapy |
Reccurence |
| 4 | 64 | F | 3 months | Nasal obstruction Epistaxis anosmia exophtalmos cervical lymphadenopathy |
Stage C | Surgery radiation therapy |
Evolutionary pursuit |
| 5 | 63 | F | 4 months | Nasal obstruction nasal sinus pains | Stage C | Palliative radiation therapy Palliative chemotherapy | Passed away |
| 6 | 27 | F | 7 months | Nasal obstruction Epistaxis Low visual acquity |
Stage C | Surgery radiation therapy |
Full remission |
Table 1. Summary of observations
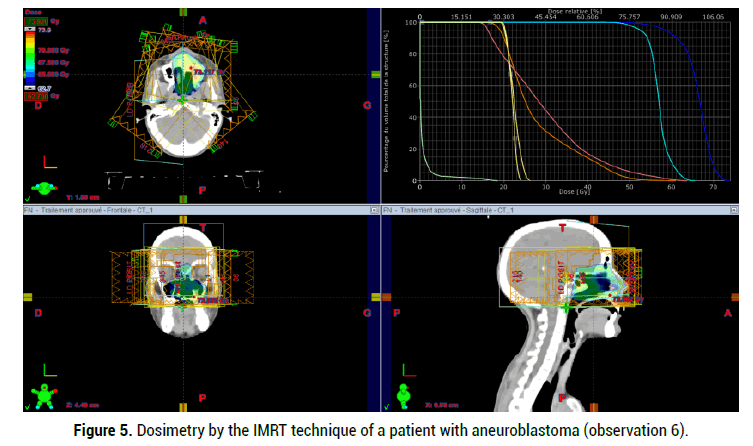
Figure 5: Dosimetry by the IMRT technique of a patient with aneuroblastoma (observation 6).
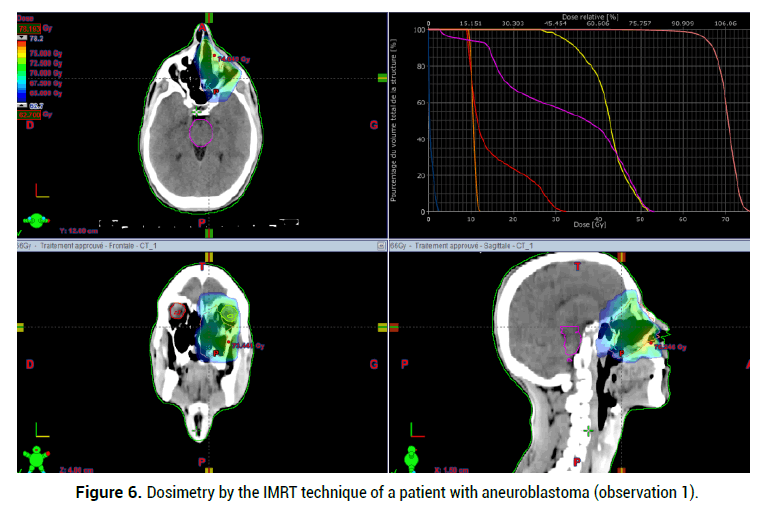
Figure 6: Dosimetry by the IMRT technique of a patient with aneuroblastoma (observation 1).
A evolutionary pursuit was noted in 1 case: 3 months after the exclusive surgical treatment. A tumor recurrence occured in 2 cases, and one patient got out of the hospital and passed away later. Table 1 summaries the observations of our patients.
The olfactory esthesioneuroblastoma was first described by Berger, et al. Therafter, 1000 cases were noted in the literature [2]. It is a rare tumor that represents 1%-2% of the overall malignat nasal sinus pains and 3% to 6% of all the nasal tumors [1,2,3,5]. The increase of the cases published during the post years corresponds more with the rise of the disease frequency [6]. In most series this tumor effects also sexes. Even if some authors report a slight female predominance [6]. The disease occurs at any age, but two frequency peaks was described between the age of 10 and 20, and between 50 and 60 [3,5,7]. No risk factor was clearly identified in the literature. However, some studies evoked a possible role of Nitrosamines, wood dust and some genetic abnormalities [8]. The initial clinical symptoms of tumours of the facial bones, including ENB, are often nonspecific [9]. The symptoms most commonly reported in the literature are identical to those described in our study [10,11].
The imaging of this type cancers essentially acquires the CT scan and the MRI which are complementary [12]. The scan, with coronal and axial images before and after the injection of contrast agent, is considered to be prefferd axamination to show a dense homogeneous opacity that might cantain intra tumoral calcifications and which moderately increase after the injection of the contrast agent [5]. Precising the exact limits of the intra cranial expansion and detectins the invasion of the anterir section [2,5]. Depending on the expansion, Kadish proposed a clinical classification in 3 stages [1,2,13].
• Stage A: Tumor limited to the nasal cavity
• Stage B: Tumor limited to the nasal cavity and the sinuses
• Stage C: Tumor extended beyon the nasal cavities and sinuses.
This classification was modified by Monita. Most recently, Dulguerov proposed a more precise classificationbasedon the TNM classification and using the CT scan and MRI [9,13].
• T1: Nasal and / or sinus tumor, keeping an air space between the tumor and cribriform plate.
• T2: Tumor touching and even eroding the cribriform plate.
• T3: Intracranial extradural tumor and/ or an orbital damage.
• T4: Intracranial intradural tumor.
The current recommended classification are one of Kadish modified by Morita, and the other of Dulguerov [7,12]. In our series, the radiological staging was done according to the classification of Kadish. Thus, 5 patients were classified stage C and a patient was stage D. The diagnosis of the esthesioneublastoma raised by the imaging, is histological [12], and it is based on the morphology and immunohistochemistry. The treatment of the esthesioneuroblastoma is proposed depending on its ability to be surgically removable, a complete resection surgery, macroscopic and microscopic, with safetymargins, followed by a radiotherapy of the tumor site and the first node bridges, which is considered to the standard curative treatment of sinus esthesioneuroblastoma (Grade C recommendation) [12]. There is no standard access, still any surgical access should take into consideration two aims [14], on the one hand, the ability to control all the anatomical limits of the tumor and the cribrifom plate; on the other hand a one piece cardcinological resection that -if possible- avoids the tumor fragmentation or the sectioning [14].
If there is an orbital extension, the attitudes are extremly nuanced but the majority of surgeons have a conservative approach toward the eyeball; since there is no significant difference in case of exenteration on survival or recurrence rates. If the tumor cannot be surgically removed, the treatment is multimodal and includes a first line chemotherapy, and an eventual radiation therapy followed by a craniofacial surgery (professional consensus) [5]. The preoperative radiotherapy, eventhough adopted by some canters, is most standard [3,7]. This radiation therapy targets the tumor site as well as lymph node area the radiation dose might be 45 Gy to 60 Gy if the tumor volume is important [15]. The olfactory esthesioneuroblastoma is a tumor white a very poor prognosis, the survivais about 50% of 5 years and 30% of 10 years. The local and locoregional recurrences represent 60% [16], and they might be early or late, which justifies a life long supervision of the patients.
The prognosis factors of the esthesioneuroblatomas are very blurring bacause of the small number of patients in every series. The main prognosis factor is the clinical stage of the diagnosis. Age, gender, and ethnicity were not noted as prognosis factors. The Hyams histological grade seems also to be a significant prognosis factor with a 56% service rate for the low grades I and II versus a 25% rate for higher grades III and IV. The other factors are presented by TNM stage and the treatment; in fact, the survival, when associating surgery and radiation therapy, is higher than the case of using only radiotherapy or isolated surgery.
Most of the patients of ENB present in locally advanced stage and the optimal management depends on the cooperation between clinicians, surgeons, radiologists and pathologists from establishing diagnosis to organizing the therapeutic strategy. Novel strategies including combined CCT with RT and/ or dose escalation with advanced RT techniques such as IMRT and proton therapy should be prospectively investigated to improve the survival results in ENB.
Citation: Amina B, et al. Olfactory Esthesioneuroblastoma: Study of 6 Cases and Review of the Literature. Med Rep Case Stud, 2021, 06(S4), 008-012
Received: 15-Sep-2021 Published: 06-Oct-2021, DOI: 10.35248/2572-5130.21.s4.008-012
Copyright: © 2021 Amina B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO