Case Report - (2021) Volume 12, Issue 11
Systemic lupus erythematosus (SLE) is known to be a multisystem autoimmune disorder. Neuropsychiatric manifestations of systemic lupus erythematosus (SLE) are heterogenous and complex. Posterior reversible encephalopathy syndrome (PRES) and its association with SLE has increasingly, been recognized. PRES as an initial manifestation of SLE is not widely reported in the literature. A case control study reported prevalence of PRES in SLE as much as 0.43%. Common presentations include headache, vomiting, altered mental function, visual symptoms, and seizures. Diagnosis is supported by classical symptoms and typical radiological feature of bilateral posterior subcortical brain edema on magnetic resonance imaging (MRI). PRES is linked with accelerated hypertension, renal impairment, eclampsia, pre-eclampsia, sepsis, cytotoxic therapy, underlying autoimmune diease, and immunosuppressive therapy. Objectives: To study the clinical profile of posterior reversible encephalopathy syndrome (PRES) in systemic lupus erythematosus (SLE) patient and determine the risk factors associated with it.Case presentation: A 26 year old Filipino female diagnosed with SLE. Overall, the disease was not well controlled due to patients non-compliance to therapy. She was brought to the emergency department due to sudden generalized tonic-clonic seizure episode. Cranial MRI revealed posterior reversible encephalopathy syndrome (PRES) and was admitted. Conclusion: PRES occurs in young lupus patients and in the early part of the disease. Focal deficits are not uncommon. It can be the presenting manifestation of lupus. Management is predominantly symptomatic. Immunosuppression is directed by other major organ manifestations. Early diagnosis and appropriate management is productive. Systemic lupus erythematosus should be considered in the differential diagnosis of patients who present with PRES. One should have a low threshold for magnetic resonance imaging especially when neurological symptoms occur in young women with or without an established diagnosis of SLE and especially among those with active SLE, lupus nephritis, renal failure, and/or poorly controlled hypertension. Given the good prognosis of PRES in SLE patients with early supportive treatment, prompt recognition is crucial to institute appropriate management.
Posterior reversible encephalopathy syndrome (PRES) is a rare, recently described neurologic condition identifiable by clinical presentation and magnetic resonance imaging (MRI) appearance [1]. Reversible MRIS hyperintensities compatible with PRES were reported as early as 1985 by Aisen, et al in lupus patients with neuropsychiatric manifestations [2]. Later, It was described as punctate or focal high-intensity lesions suggestive of edema that resolved with corticosteroid treatment [3]. “PRES” is first described in 1996 as a neuro-radiological entity characterized by headache, altered mental function, visual disturbance, seizures and posterior transient changes on neuro-imaging [4]. Classical MRI (Magnetic resonance imaging) findings were initially described as bilateral sub-cortical hyper-intense areas involving occipital and parietal lobes although involvement of other lobes including the cerebellum have since been reported [5]. And there were four reported cases of PRES complicating systemic lupus eythematosus (SLE) [6].
Systemic Lupus Erythematosus (SLE) is a chronic multisystem inflammatory disease that follows a relapsing and remitting course. It is characterized by an auto-antibody response to nuclear and cytoplasmic antigens. SLE can affect any organ system, but mainly involves the skin, joints, kidneys, blood cells, and nervous system [7]. PRES as an initial manifestation of SLE is not widely reported in the literature. A case control study reported prevalence of PRES in SLE as much as 0.43% [8]. PRES is completely reversible with blood pressure control and supportive measures; immunosuppression is indicated only for treating the underlying active SLE.
A case of a 26 year old female, Filipino, presented with generalized tonicclonic seizure. She was apparently well, until 1 hour prior to admission she was seen in bed witnessed by a relative to have sudden loss of consciousness associated with stiffening of all extremities and upward rolling of the eyeballs, bluish discoloration of the lips lasting for about a minute. She was brought immediately to the emergency room where she regained consciousness 1 hour later and complained of generalized headache which she was not able to describe due to drowsiness and confusion.
Six months prior to admission, she started to develop facial maculopapular rashes, which was attributed to allergies. At the same year, she developed bipedal edema associated with puffy eyelids and dysuria. There were no investigations conducted to confirm the diagnosis.
2 weeks prior to admission, she was admitted at a local hospital for suspected SLE. Pulse therapy with methylprednisolone was initiated following the confirmation of SLE. She was sent home with the following medications; Epoietin, Ketoanalogues, Hydrochloroquine, Methylprednisone, Mycophenolate, and Ferrous Sulfate + Folic acid.
On arrival to the emergency department, she was noted to be hypertensive with BP of 190/120 mmHG. This was treated acutely with intravenous Nicardepine, which resulted in short term reduction in blood pressure. She then had a second witnessed generalized tonic-clonic seizure and was given intravenous Diazepam. On examination, HR=92, RR=21, T=36 C and Oxygen saturation of 96% at room air. She was drowsy, weak looking and tachypneic. The pupils measured 2-3 mm and reactive to light. Eyeballs were moving in all directions, there was no facial asymmetry or any focal motor or sensory deficits. Neck was supple, palpebral conjunctivae was pale, there was a malar rash on her face, hair strands were seen to be thin and an area of alopecia was seen on the frontal hairline. Neck stiffness was absent. There was no lymphadenopathy. Chest expansion was symmetrical, there was no intercostal retraction and the lungs were clear. The cardiac PMI was not deviated, there was no murmur and the cardiac rhythm was regular. There was Grade II pitting bipedal edema.
A Cranial MRI was performed, revealed a diffuse patchy hyperintensity changes in fronto-parietal and basal ganglia regions, presumably ischemic in origin of which cerebral vasculitis is the main consideration. Findings in both occipital lobes consistent with posterior reversible encephalopathic syndrome. There was no intracranial mass nor hemorrhage. Lumbar puncture was not done. She was referred to a Neurologist and was given a bolus of intravenous valproic acid, a provisional diagnosis of Neuropsychiatric SLE on the background of PRES finding on cranial MRI. An Electro Encephalogram (EEG) was requested but was not done due to patients financial status. Based on the clinical presentation and imaging changes, a diagnosis of Posterior Reversible Encephalopathy Syndrome (PRES) was made due to undiagnosed hypertension. She was allowed to continue her regular home medicines which included the following: EPO A 4000u SQ once a week, Ketoanalogues 600mg tab, 2 tabs TID, Nephrocan HP 1 cap every other day, Hydroxychloroquine 200mgtab OD, Methylprednisolone 16mg tab OD, Mycofenolate mofetil 500mg tab BID, FeSO4 + FA tab TID.
Oral valproic acid was commenced for seizure control and oral losartan for management of blood pressure, which was up to 190/120. She continued to receive intermittent intravenous nicardepine and continued oral anti-hypertensive medication. 24 hours after admission, there was no recurrence of seizure and BP elevations was controlled. However, on examination she was seen to have weakness on left upper and lower extremities graded as 2/5 with no associated sensory deficits interpreted as part of the neurological complications of SLE in flare as seen evident on brain MRI as pres. Which motor strength eventually improved to 5/5 on the next 5 days.
Further investigations revealed a lupus panel results from previous admission, a immunofluorescent ANA elevated at 160, markedly elevated dsDNA antibody level of >226, elevated Anti SnRNP, Anti Smith, Anti SSA, CRP. A diagnosis of Systemic Lupus Erythematosus was made, 1st dose of cyclophosphamide was infused and methylprednisolone was instituted with clinical and blood pressure improvement (Table 1).
| REFERENCE RANGE | RESULT | |
|---|---|---|
| CRP | 0.00 – 10.0 mg/dL | 16.4 H |
| Urine Protein/Creatinine Ratio | <22.60 ug/mmol | 1448.36 ug/mmol |
| Anti- Cardiolipin antibodies igG/IgM | Negative | |
| LE PANEL | ||
| ANA Immunofluorescent | 160 H | |
| Anti DSDNA | >200: strongly Positive | >226.76 |
| ANTI ENA PANEL | ||
| Anti SnRNP | >18: Positive | 48.80 |
| Anti Smith | >18: Positive | 19.50 |
| Anti SSA | >18: Positive | 90.60 |
| Anti SSB/La | <12: Negative | <3.0 |
| Anti Jo-1 | <12: Negative | <3.0 |
Table 1: Laboratory Results.
Subsequent directed history from family member revealed a 6 month history of facial maculopapular rashes which was attributed to allergies. At the same year, she developed bipedal edema associated with puffy eyelids, mild alopecia was also noted. There was no history of Arthritis, miscarriage or thromboembolism. She also had no previous history of hypertension. There were no investigations conducted to confirm the diagnosis.
The patient’s condition improved gradually; there was no further seizure. Due to elevated creatinine, HP/HD was done and a renal biospsy was requested due to the presence of proteinuria (>0.5mg/24 hrs) and persisting microscopic hematuria attributed to lupus nephritis. However it was not done due to lack of finances. Prior to discharge, she was commenced on methylprednisolone 16mg tab thrice a day, oral hydroxychloroquine was continued. The patient has shown response with no further neurological symptoms and a follow-up instruction and medications were given (Figure 1) (Table 1).
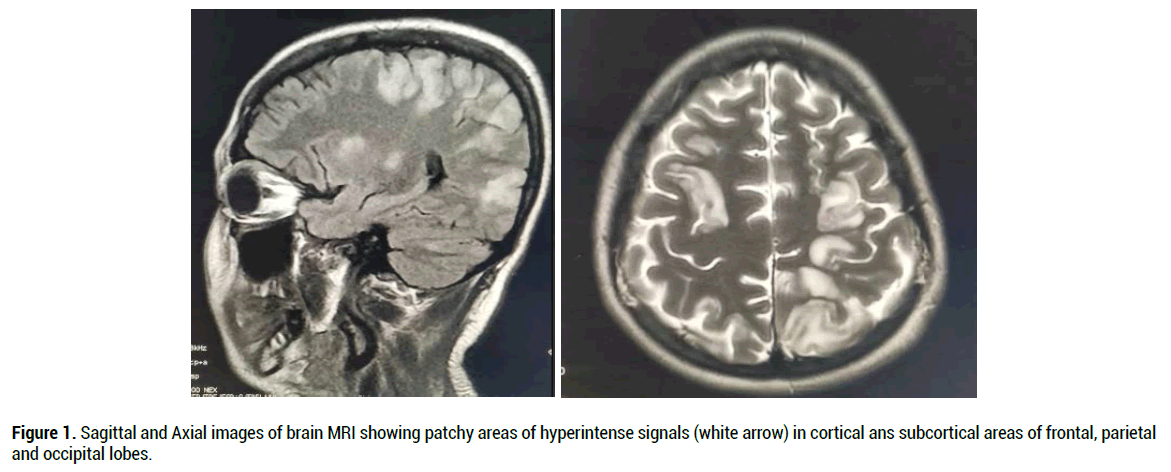
Figure 1. Sagittal and Axial images of brain MRI showing patchy areas of hyperintense signals (white arrow) in cortical ans subcortical areas of frontal, parietal and occipital lobes.
This study shows that PRES can be the presenting manifestation of SLE, where patients tend to present in the early stage of the disease. Headaches and seizures were the most common manifestations and patients had active lupus, with lupus nephritis being the most common accompaniment and that hypertension is most often mild. The proposed pathogenic mechanisms are disordered cerebral autoregulation and endothelial dysfunction.
Posterior Reversible Encephalopathy Syndrome (PRES) is also known as reversible posterior leukoencephalopathy syndrome that is characterized by brain imaging that includes vasogenic edema and clinical symptoms of hypertension, headache and seizure [9]. While other previous studies define PRES as a development in association with hypertension, renal disease, autoimmune disorders, and treat with cytotoxic drugs and that systemic lupus erythematosus (SLE) is one of the predisposing condition conditions related to PRES, particularly when accompanied by lupus nephritis [10]. PRES has been described in association with systemic vasculitis, thrombotic thrombocytopenic purpura, haemolytic uraemic syndrome, infection and other miscellaneous conditions [7]. PRES has also been described in association with number of immnunosuppressive and cytotoxic agents including corticosteroids, cyclophosphamide, mycophenolate and rituximab [11].
Systemic lupus erythematosus (SLE) is a connective tissue autoimmune disease characterized by a broad spectrum of clinical manifestations [12]. It is commonly presents with arthritis, glomerulonephritis, serositis, cutaneous, hematological, and nervous system manifestations [13]. The prevalence of PRES as an initial manifestation of SLE is not widely reported in the literature [14].
PRES in SLE commonly affects the female, with a median age of onset ranging from 9-82 year. It was also highlighted in one of the study made by Fugate et al. the prevalence of signs and symptoms in 113 patients with PRES and reported that seizure was the most common symptom, followed by encephalopathy, headaches, and visual disturbances [15]. However, data of seizures as an initial manifestation of SLE is lacking. Our patient is diagnosed SLE who presented with seizure episode and a PRES syndrome on cranial MRI.
The pathophysiology of PRES in SLE remains unclear. The classical understanding is that an acute rise in blood pressure exceeds the autoregulation of cerebral circulation, leading to increased cerebral blood flow and hyperperfusion brain injury. On the contrary, an excessive autoregulation response may cause a focal cerebreal vasoconstriction, leading to brain ischaemia. The attribution to hypertensive crisis may explain part of the pathophysiology. However, the mechanism of PRES is unlikely explained by hypertension alone. Several cases of PRES in patients with SLE with normal blood pressure have been reported [16].
Our patient was diagnosed with SLE based on the American College of Rheumatology (ACR) criteria [17] and EULAR new classification criteria where she scored 38 points indicating presence of active SLE (see Appendix).
PRES may occur anytime in the disease course of lupus. Seizures and headaches were the most common presenting features which was explained by the diffuse expression of lesions and cortical involvement seen on cranial MRI as well as the diffuse edema causing headache. PRES should always be a differential diagnosis in acute headache and that renal failure and severe hypertension are known risk factors for the development of PRES but there are case reports of PRES in normotensive patients with SLE were ascribed to high doses of corticosteroids or to cytotoxic therapy with cyclophosphamide. The mainstay of treatment is supportive control of BP and seizures by giving anti hypertensive and anti seizure drugs, withdrawal of offending drug and directed treatment of systemic SLE activity including corticosteroids and cyclophosphamide. Balance of treatment is important for immunosuppresion management of disease activity against the risk of immunosuppression-associated disease or relapse. Multiple etiologies may be responsible for occurrence of PRES in SLE patients already undergoing treatment with cytotoxic therapy. PRES is considered benign and complete recovery can be expected, residual deficits are not uncommon, as noted in our patient in the form of hemiparesis. The management is predominantly symptomatic.
Citation: Daphne Angelie Sevilleja, Posterior Reversible Encephalopathy In Systemic Lupus Erythematosus: A rare Case Report. J Neurol Neurophy, 2021, 12(11), 563.
Received: 08-Nov-2021 Published: 30-Nov-2021
Copyright: © 2021 Sevilleja DA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.