Research - (2021) Volume 11, Issue 4
Background: Globally, 50% or more of the world’s population is infected with Helicobacter pylori making it the most widely spread bacteria across the world. The low developed countries are more overburdened by Helicobacter pylori infection than the developed countries. H. pylori infection is associated with duodenal ulcer, chronic atrophic gastritis (CAG), lymphomas, and adenocarcinoma. This study reports the prevalence of H. pylori and its associated factors in Eastern Uganda.
Materials and methods: A cross-sectional study involving 275 participants was carried out in eastern Uganda. H. pylori serology was done and face to face interviewer-administered questionnaire were used for data collection. Data were entered in Microsoft Excel and imported to Stata version 14 for analysis and a P value of <0.05 was considered statistically significant.
Results: The seroprevalence of H. pylori was 27.3% (75/275) with 28.4% (50/176) of the females being positive compared to25.3% (25/99) of the males. Consumption of animal products (meat, milk, and eggs) was the only statistically significant factor associated with H. pylori seropositivity (P ˂0.001, 95% CI =1.934-4.209, AOR=2.85).
Conclusion: The H. pylori seroprevalence is high in eastern Uganda. Consumption of animal products was a positive predictor of infectivity.
Helicobacter pylori • Animal products • Seroprevalence • Kibuku • Eastern Uganda
The initial isolation of Helicobacter pylori by Marshal and Warren [1] in 1982 marked not only a critical point in understanding the gastrointestinal tract microbial ecology but also it being a pathogen in a variety of diseases including lymphomas and carcinomas [2] and extra gastrointestinal systemic diseases such as idiopathic urticaria and autoimmune thyroid disease [3]. The fact that half or more of the World’s population is infected with Helicobacter pylori makes it not only the most widely spread bacteria across the World [4] but also a public health concern. Previous studies have reported this gramnegative bacteria as a cause of chronic gastric inflammation in all infected individuals and have been associated with gastric or duodenal ulcers in 10- 55%, low-grade B-cell mucosa-associated lymphoid tissue lymphoma of the stomach (MALToma) [5] in approximately 1% [6], gastric adenocarcinoma [7], and colorectal cancer [8]. Gastric adenocarcinoma is the third leading cause of cancer deaths Worldwide [2]. Worse still, the global burden of noncardia gastric cancer attributable to H. pylori has increased from 5.2% to 6.2% of all cancers [9].
Although the transmission pathways of H. pylori to humans and its reservoirs is still an enigma, current literature suggests that the transmission of H. pylori occurs from person to person via the oral-oral, fecal-oral, and gastric-oral routes [10]. Moreover, sexual transmission has also been documented [11]. The survival of H. pylori in gastric juices is thought to be facilitated by its motility and four to six unipolar-sheathed flagella it possesses and the urease activity. Whatever the case, close contact plays a major role in transmission. Moreover, although the prevalence of H. pylori exceeds 70% in many low and medium income countries, only a small proportion of the population may develop severe symptoms [12]. In many developed countries, the prevalence of H. pylori has been declining due to improved standards of living [13]. In developing countries, a lot needs to be done to realize a decline in the prevalence of H. pylori and its complications due to low economic status.
Early and frequent screening and detection of H. pylori infection may be useful to prevent the development of severe symptoms in a population with a low socioeconomic status.
There is a dearth of literature from eastern Uganda regarding the prevalence of H. pylori and its associated factors. The objective of this study was to determine the prevalence of H. pylori and its associated factors in Kibuku district, Eastern Uganda.
Study design, area of the study and sampling
A cross-sectional study was carried out from May to July 2019 in Kibuku district. Kibuku District is one of the Community Based Education and Research Services (COBERS) sites of Busitema University (Appendix 1). Kibuku District is about 200km on the east of the capital city Kampala in Uganda and is bordered by districts; Pallisa in the north, Budaka to the east, Butaleja to the South, and Namutumba to the west with an estimated population of 202,033 [14]. Kibuku has an adult illiteracy rate of41.9%, only 29% of the population is within 5km of a public health facility,1.8% have access to piped water and only 38.7% have properdisposal of solid wastes and 99% of the population live in indecent dwellings [14]. It is envisaged that inaccessibility to safe water and improper disposal of waste are enabling factors for colonization of the gastrointestinal tract by Helicobacter pylori.
Data collection
We used the two community outreaches that had been organized to provide outreach services amongst the residents of Kibuku distrct. Kibuku has two counties; Kibuku and Kabweri. By raffle draw, Kibuku was chosen. Of the six subcountiues (Kirika, Kadama, Kabweri, Kagumu, Bulangira and Kibuku) in Kibuku, Kadama sucounty was randomly selected.We mapped out two centres that residents normally go to for outreaches and using village Health teams,outreaches were called on the same day at those different locations. We estimated these camps to attract about 800 in total. 275 participants were systematically selected (138 participants from one site and 137 from the other) to take part in this study. The residents come to these outreach centres to seek various services including HIV testing and counseling, blood pressure measurements, random blood sugar measurement and treatment of other ailments, and deworming of the children. Using the systematic random sampling, we recruited 275 attendants that had come for the outreach projects. These participants were approached and explained to about the research and for those who were 18years of age and above, written informed consent was sought while for those below informed written assent in addition to written informed consent from their adult care takers. Interviewer administered pretested face-to-face questionnaire, developed by the researchers for this study(supplementary material) was used to collect data.
Detection of H. pylori
A volume of 2ml of venous blood was collected into plain vacutainers and the serum was separated by centrifugation and used for detection of H. pylori using Healgen immunochromatographic test cards (Xiamen Biotech Co., Ltd, China) [15].
Data processing and analysis
Data collected was double entered and cleaned using Microsoft Excel and imported to Stata version 14 for analysis. Frequency distribution and two-way tables were used to summarise the data. Chi-square (2X2) was applied for the P-value derivation for socio-demographic and risk factors to determine those factors that were significantly associated with H. pylori infection. After the univariate descriptive analysis, bivariate analysis was done, and factors that were significant and or had P-value <0.05 were considered for multivariate logistic regression to further examine the association between each the dependent variable and independent variables while controlling for the confounders.
Ethical consideration
The ethical clearance letter was obtained from Busitema University Faculty of Health Sciences Community Based Education, Research and Services Committee and administrative clearance was obtained from Kibuku district. Finally, informed written consent was requested from each participant. Participants below 18 years provided written assent as per the guidelines from Uganda National Council of Science and Technology (UNCST).
The seroprevalence of H.pylori was 27.3% (75/275) (Figure 1) with 28.4% (50/176) of the females being positive compared to 25.3% (25/99) of the males.
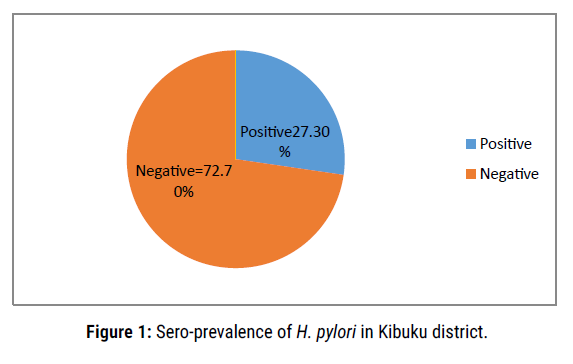
Figure 1. Sero-prevalence of H. pylori in Kibuku district
Regarding sociodemographic characteristics, the majority were females at 64% while males made up 36%. The majority were married 73.3%, while 5.1% had divorced and 6.2% lost a spouse. Education level was generally low with 54.5% having gone to primary while 9.3% were illiterate. Furthermore, the parents were lowly educated with 84.6% and 94.1% of the mothers and fathers respectively being either illiterate or ended in primary school. Moreover, 64.5% reported a history of gastrointestinal (GIT) disease in the family while 62% reported GIT disease in themselves. Further, still, 57.1% reported the use of antibiotics in relation to ulcers in the last one month. On bivariate analysis, no factor was significantly associated with H. pylori infection. (Table 1).
| Demographic characteristics | Frequency (%) | H. Pylori infection | P-value | |
|---|---|---|---|---|
| Negative | Positive | |||
| Sex | N (%) | N (%) | 0.573 | |
| Female | 176 (64) | 126 (63) | 50 (66.7) | |
| Male | 99 (36) | 74 (37) | 25 (33.3) | |
| Total | 275 (100) | 200 (100) | 75 (100) | |
| Age group | 0.128 | |||
| 13-24years | 42 (15.3) | 35 (17.5) | 7 (9.3) | |
| 25-36 | 79 (28.7) | 51 (25.5) | 28 (37.3) | |
| 37-48 | 75 (27.3) | 55 (27.5) | 20 (26.7) | |
| 49-60 | 50 (18.2) | 40 (20) | 10 (13.3) | |
| Above 60 years | 29 (10.5) | 19 (9.5) | 10 (13.3) | |
| Total | 275 (100) | 200 (100) | 75 (100) | |
| Marital Status | 0.361 | |||
| Divorced | 14 (5.1) | 12 (6) | 2 (2.7) | |
| Loss of Spouse | 17 (6.2) | 11 (5.5) | 6 (8.1) | |
| Married | 202 (73.7) | 144 (72) | 58 (78.4) | |
| Unmarried | 41 (15) | 33 (16.5) | 8 (10.8) | |
| Total | 274 (100) | 200 (100) | 74 (100) | |
| Education level | 0.578 | |||
| A-level | 5 (1.8) | 4 (2) | 1 (1.3) | |
| Illiterates | 26 (9.5) | 21 (10.5) | 5 (6.7) | |
| O-level | 83 (30.2) | 61 (30.5) | 22 (29.3) | |
| Primary | 150 (54.5) | 108 (54) | 42 (56) | |
| Tertiary | 11 (4) | 6 (3) | 5 (6.7) | |
| Total | 275 (100) | 200 (100) | 75 (100) | |
| The education level of Father | 0.777 | |||
| Illiterates | 26 (10.2) | 20 (10.7) | 6 (9) | |
| O-level | 24 (9.4) | 18 (9.6) | 6 (9) | |
| Primary | 196 (77.2) | 142 (75.9) | 54 (80.6) | |
| Tertiary | 8 (3.1) | 7 (3.7) | 1 (1.5) | |
| Total | 254 (100) | 187 (100) | 67 (100) | |
| Education of Mother | 0.39 | |||
| Illiterates | 38 (15) | 30 (16.1) | 8 (11.9) | |
| O-level | 10 (4) | 8 (4.3) | 2 (3) | |
| Primary | 200 (79.1) | 143 (76.9) | 57 (85.1) | |
| Tertiary | 5 (2) | 5 (2.7) | 0 (0) | |
| Total | 253 (100) | 186 (100) | 67 (100) | |
| Annual Income(Uganda shillings) | 0.679 | |||
| ≤ 500,000 | 159 (60.2) | 117 (60.9) | 42 (58.3) | |
| 500,000-1million | 57 (21.6) | 38 (19.8) | 19 (26.4) | |
| 2m-3million | 40 (15.2) | 30 (15.6) | 10 (13.9) | |
| 4m-5million | 6 (2.3) | 5 (2.6) | 1 (1.4) | |
| 5-6million | 2 (0.8) | 2 (1) | 0 (0) | |
| Total | 264 (100) | 192 (100) | 72 (100) | |
| History of gastrointestinal disease in the family | 0.713 | |||
| No | 97 (35.5) | 72 (36.2) | 25 (33.8) | |
| Yes | 176 (64.5) | 127 (63.8) | 49 (66.2) | |
| Total | 273 (100) | 199 (100) | 74 (100) | |
| History of gastrointestinal disease in the individual | 0.208 | |||
| No | 103(38.0) | 79(40.3) | 24(32.0) | |
| Yes | 168(62.0) | 117(59.7) | 51(68.0) | |
| Total | 271(100) | |||
| Use of antibiotics in relation to ulcers in the last one month | 0.757 | |||
| No | 66(42.9) | 106 (58.9) | 36 (54.5) | |
| Yes | 88(57.1) | 74 (41.1) | 30 (45.5) | |
| Total | 154 (100) | 110 (100) | 44 (100) | |
Table 1: Relationship between demographic characteristics of the 275 participants and H. pylor iseroprevalence in Kibuku district.
Regarding hygiene practices, 99.6 % reported washing hands before a meal of whom 80.1% reported using soap and water. Furthermore, 98.1% reported washing hands after visiting a latrine. Whereas only 5.6% used cutlery during eating, 65.2% shared it. Further, still, 96% of the study participants reported not washing fruits and vegetables before eating them. The majority, 93% did not share housing with animals or poultry. On bivariate analysis, what one washed hands with was significantly associated with H.pylori infection (P=0.029) (Table 2).
| Hygiene applications | Frequency (%) | H. Pylori infection | P-value | |
|---|---|---|---|---|
| Negative | Positive | |||
| Share materials such as forks, spoons, and knife with others | N (%) | N (%) | 0.154 | |
| No | 93 (34.8) | 63 (32.3) | 30 (41.7) | |
| Yes | 174 (65.2) | 132 (67.7) | 42 (58.3) | |
| Total | 267 (100) | 195 (100) | 72 (100) | |
| Wash hands before a meal | 0.102 | |||
| No | 1 (0.4) | 0 (0) | 1 (1.3) | |
| Yes | 274 (99.6) | 200 (100) | 74 (98.7) | |
| Total | 275 (100) | 200 (100) | 75 (100) | |
| Wash hands with | 0.029 | |||
| None | 2 (1) | 0 (0) | 2 (3.8) | |
| Soap & Water | 165 (80.1) | 122 (79.2) | 43 (82.7) | |
| Water | 39 (18.9) | 32 (20.8) | 7 (13.5) | |
| Total | 206 (100) | 154 (100) | 52 (100) | |
| Wash hands after using a latrine/toilet | 0.532 | |||
| No | 5 (1.9) | 3 (1.5) | 2 (2.7) | |
| Yes | 263 (98.1) | 191 (98.5) | 72 (97.3) | |
| Total | 268 (100) | 194 (100) | 74 (100) | |
| The cutlery used to eat food | 0.721 | |||
| Fork | 14 (5.2) | 11 (5.6) | 3 (4.1) | |
| Hands | 255 (94.4) | 184 (93.9) | 71 (95.9) | |
| Spoon | 1 (0.4) | 1 (0.5) | 0 (0) | |
| Total | 270 (100) | 196 (100) | 74 (100) | |
| Wash vegetables and fruits before eating them | 0.361 | |||
| No | 10 (4) | 6 (3.3) | 4 (5.8) | |
| Yes | 242 (96) | 177 (96.7) | 65 (94.2) | |
| Total | 252 (100) | 183 (100) | 69 (100) | |
| Share housing with animals/poultry | 0.333 | |||
| No | 252 (93) | 185 (93.9) | 67 (90.5) | |
| Yes | 19 (7) | 12 (6.1) | 7 (9.5) | |
| Total | 271 (100) | 197 (100) | 74 (100) | |
Table 2: Relationship between hygiene practices of the 275 participants and H. pyloriseroprevalence in Kibuku district.
We further explored the association between history of smoking, drinking alcohol, and H. pylori infection. Significantly only 2.7% smoked tobacco and of those that smoked only 20% smoked more than 15 sticks of cigarettes per day. Moreover, only 50% had smoked for 10-15 years. As regards alcohol intake only 7% consumed alcohol. However, in bivariate analysis, no factor was significantly associated with alcohol smoking or alcohol intake (Table 3).
| History of smoking and drinking | Frequency (%) | Helicobacter Pylori infection | P-value | |
|---|---|---|---|---|
| Negative | Positive | |||
| Smoking of cigarettes | 0.934 | |||
| No | 265 (97.4) | 193 (97.5) | 72 (97.3) | |
| Yes | 7 (2.6) | 5 (2.5) | 2 (2.7) | |
| Total | 272 (100) | 198 (100) | 74 (100) | |
| Number of cigarettes per day | 0.659 | |||
| 1 to 5 | 3 (60) | 2 (50) | 1 (100) | |
| 6 to 10 | 1 (20) | 1 (25) | 0 (0) | |
| >15 | 1 (20) | 1 (25) | 0 (0) | |
| Total | 5 (100) | 4 (100) | 1 (100) | |
| Duration of smoking | 0.513 | |||
| 1 to 5 | 1 (25) | 1 (33.3) | 0 (0) | |
| 11 to 15 | 2 (50) | 1 (33.3) | 1 (100) | |
| >15 | 1 (25) | 1 (33.3) | 0 (0) | |
| Total | 4 (100) | 3 (100) | 1 (100) | |
| Drinking of alcohol | 0.941 | |||
| No | 251 (93) | 183 (92.9) | 68 (93.2) | |
| Yes | 19 (7) | 14 (7.1) | 5 (6.8) | |
| Total | 270 (100) | 197 (100) | 73 (100) | |
| Quantity of alcohol consumed per day | 0.641 | |||
| 0-200 | 10 (55.6) | 7 (50) | 3 (75) | |
| 201-500 | 7 (38.9) | 6 (42.9) | 1 (25) | |
| 3 Bottles | 1 (5.6) | 1 (7.1) | 0 (0) | |
| Total | 18 (100) | 14 (100) | 4 (100) | |
| Type of alcohol taken | 0.258 | |||
| Beer & Waragi (local liquor) | 7 (41.2) | 6 (46.2) | 1 (25) | |
| Local | 7 (41.2) | 4 (30.8) | 3 (75) | |
| Malwa | 3 (17.6) | 3 (23.1) | 0 (0) | |
| Total | 17 (100) | 13 (100) | 4 (100) | |
| Duration of drinking alcohol | 0.737 | |||
| 1 to 5 | 5 (29.4) | 3 (23.1) | 2 (50) | |
| 11 to 15 | 1 (5.9) | 1 (7.7) | 0 (0) | |
| 16-20 | 3 (17.6) | 2 (15.4) | 1 (25) | |
| 6 to 10 | 2 (11.8) | 2 (15.4) | 0 (0) | |
| >20 | 6 (35.3) | 5 (38.5) | 1 (25) | |
| Total | 17 (100) | 13 (100) | 4 (100) | |
Table 3: Relationship between history of smoking, drinking alcohol consumption of the study participants and H. pylori seroprevalence in Kibuku district.
Regarding dietary intake and H. pylori infection, 28.3% and 27.8% ate greens and fruits every day. Moreover, only 12% ate animal products every day. Furthermore, 1.8% reported not eating beans while 98.2% that eat, 71.3% did not eat them daily. The participants reported that their main source of water was borehole, 92.4% while only 0.7% accessed piped water. Significantly only 18.2% boiled water for drinking while a further 33.3% reported treating it using water guard. On bivariate analysis, the only significant factor associated with H. pylori infection was feeding on animal (meat, eggs, and milk) products (P=0.045)(Table 4).
| Dietary intake | Frequency (%) | Helicobacter Pylori infection | P-value | |
|---|---|---|---|---|
| Negative | Positive | |||
| How often do you eat greens | 0.85 | |||
| Every Day once a day | 53 (19.5) | 37 (18.7) | 16 (21.6) | |
| More than once everyday | 24 (8.8) | 18 (9.1) | 6 (8.1) | |
| Not Everyday | 195 (71.7) | 143 (72.2) | 52 (70.3) | |
| Total | 272 (100) | 198 (100) | 74 (100) | |
| How frequently do you eat fruits | 0.446 | |||
| Everyday once a day | 61 (22.3) | 41 (20.6) | 20 (26.7) | |
| More than once everyday | 15 (5.5) | 10 (5) | 5 (6.7) | |
| Not Every Day | 198 (72.3) | 148 (74.4) | 50 (66.7) | |
| Total | 274 (100) | 199 (100) | 75 (100) | |
| How frequently do you take milk, meat, and eggs | 0.045 | |||
| Everyday once a day | 31 (11.3) | 22 (11) | 9 (12.2) | |
| More than once everyday | 2 (0.7) | 0 (0) | 2 (2.7) | |
| Neither of the above | 7 (2.6) | 7 (3.5) | 0 (0) | |
| Not Every Day | 234 (85.4) | 171 (85.5) | 63 (85.1) | |
| Total | 274 (100) | 200 (100) | 74 (100) | |
| How frequently do you eat beans | 0.724 | |||
| Does not eat | 5 (1.8) | 4 (2) | 1 (1.4) | |
| Everyday once a day | 61 (22.4) | 41 (20.7) | 20 (27) | |
| More than once everyday | 12 (4.4) | 9 (4.5) | 3 (4.1) | |
| Not everyday | 194 (71.3) | 144 (72.7) | 50 (67.6) | |
| Total | 272 (100) | 198 (100) | 74 (100) | |
| What do you use to eat your food | 0.721 | |||
| Fork | 14 (5.2) | 11 (5.6) | 3 (4.1) | |
| Hands | 255 (94.4) | 184 (93.9) | 71 (95.9) | |
| Spoon | 1 (0.4) | 1 (0.5) | 0 (0) | |
| Total | 270 (100) | 196 (100) | 74 (100) | |
| How frequently do you eat fried foods | 0.476 | |||
| Does not eat | 2 (0.7) | 2 (1) | 0 (0) | |
| Everyday once a day | 51 (18.8) | 38 (19.2) | 13 (17.6) | |
| More than once everyday | 72 (26.5) | 48 (24.2) | 24 (32.4) | |
| Not everyday | 147 (54) | 110 (55.6) | 37 (50) | |
| Total | 272 (100) | 198 (100) | 74 (100) | |
| How frequently do you eat hot food | 0.361 | |||
| Everyday once a day | 47 (17.3) | 37 (18.9) | 10 (13.3) | |
| More than once a day | 86 (31.7) | 58 (29.6) | 28 (37.3) | |
| Not everyday | 138 (50.9) | 101 (51.5) | 37 (49.3) | |
| Total | 271 (100) | 196 (100) | 75 (100) | |
| Drinking water source | ||||
| What is your source of drinking water | 0.634 | |||
| Borehole | 254 (92.4) | 186 (93) | 68 (90.7) | |
| Piped Water | 2 (0.7) | 1 (0.5) | 1 (1.3) | |
| Shadoof | 6 (2.2) | 5 (2.5) | 1 (1.3) | |
| Spring | 13 (4.7) | 8 (4) | 5 (6.7) | |
| Total | 275 (100) | 200 (100) | 75 (100) | |
| How do you handle drinking water | 0.264 | |||
| Boiling | 41 (18.2) | 28 (17.1) | 13 (21.3) | |
| None/unboiled/untreated | 109 (48.4) | 86 (52.4) | 23 (37.7) | |
| Treatment(Water Guard) | 75 (33.3) | 50 (30.5) | 25 (41) | |
| Total | 225 (100) | 164 (100) | 61 (100) | |
Table 4: Relationship between dietary intake demographic characteristics of the study participants and H. pylori seroprevalence in Kibuku district.
On logistic regression, the only statistically significant factor associated with H. pylori was the frequency with which one fed on animal (meat, milk, and eggs) products (P <0.001 95%CI 1.934-4.209, AOR=2.85). Consumption of these products more than once every day was more protective than not taking them every day with the later 2.85 times more likely to have H. pylori infection compared to the former.
Although what one washed their hands with was not statistically significant in relation to H. pylori infection (P=0.236, 95%CI 0.701-4.217 AOR=1.72), washing with water and soap was protective compared to using only water with the later having odds of 1.72 (Table 5).
| Predictor factors | Adjusted odds Ratio | P>z | [95% Conf. | Interval] |
|---|---|---|---|---|
| Wash hands wash with: | ||||
| Water and soap | 1 | |||
| Water | 1.72 | 0.236 | 0.701 | 4.217 |
| How frequently do you take milk, meat, and eggs | ||||
| More than once every day | 1 | |||
| Not Every Day | 2.85 | 0.001 | 1.934 | 4.209 |
Table 5: Multivariate analysis of the predictive factors of study participants and H. pylori seroprevalence in Kibuku district.
The overall H. pylori seroprevalence was 27.3% with females more affected at 66.7% compared to 33.3% for males. This was lower than the seroprevalence of 31.6% in Mbarara (Phoebe Aitila, 2019) and 37.4% in Kasese [16]. The difference can be attributed differences in the study participants, the geographical region, and the economic activities. Western Uganda is awash with cattle keeping whereas in the Eastern region people majorly cultivate land. H. pylori has been shown to survive better in animal products below room temperature [17].
Furthermore, theprevalence in the current studywas lower than those reported in other studies elsewhere in Sub-Saharan Africa such as 39.1% in Tanzania [18], 36.8% in Ethiopia [19], and at 51.5- 64.39% in Cameroon [20]. In Cameroon, Laure et al. [21] found a prevalence of 64.39% from a largely urban population in the country’s capital and commercial city. This could largely be due to the inherent nature of the poor sanitation and pollution that characterizes most urban centers in comparison to the rural setting village. Studies by Abera et al. [19] in Ethiopia in 2019 and Hyasinta et al. [18] in Tanzania in 2016 recruited patients from specialized clinics in hospitals who are likely to have higher seroprevalence compared to those in the current study.
A related study conducted in Asia amongst children,the seroprevalence was 49.8% [22]. In Riyadh Saudi Arabia, the prevalence was lower at 10.2% [23] while it was 11.5% in Tanzania [24].The difference could be attributed to the differences in the study population,geographical location, the methodology and nutrition.
In this study,the seroprevalence appears to increase with age though this was not statistically significant. In agreement with our study, a studies in Ethiopia [19] and Tanzania [24] showed that age was not statistically significant predictor of H. pylori seroprevalence. In contrast to findings in this study, a studies in Saudi Arabia [22] and in Augsburg, Germany [25], found age as a statistically significant predictor of H. pylori infection.
In thisstudy, the only statistically significant factor associated with H. pylori seroprevalence was the frequency with which one fed on animal (meat, milk, and eggs) products (P <0.001 , 95%CI 1.934-4.209, AOR= 2.85). The fact that consumption of animal foods was significant can be explained by H. pyloriintrinsic ability to survive in artificially contaminated milk stored at 4°C for several days (from 5 to 9 days in pasteurized milk and from approximately 6 to 12 d in sterile milk) for approximately 7 days in ground beef at 4°C, up to 3 days at -18°C [17]. Moreover H. pylori has been found in chicken products [26].
Eating greens was not found significantly affecting seropositivity. Moreover, survival time in vegetables is shorter than in animal foods; 3 days in sanitized lettuce and carrot stored at 8°C, 4 days in sterilized carrot and 5 days in carrot packaged in a modified atmosphere [27] probably due to exposure of this none-robust bacteria to oxygen and desiccation on the surface of vegetables in contrast to what happens in liquid food in which a high bacteria load is favoured [28]. However this does not mean that vegetables are not inhabited due to the potential of the bacteria to form a biofilm [29] Carrots and lettuce are rarely a delicacy in this study area.
The level of education was not a significant factor in positivity. This was in agreement with a study in Ethiopia that showed that although no formal education and having completed the tertiary level increased the odds, there were not statistically significant [30]. This finding was further in agreement with a study in Tanzania [18]. However in contrast to findings in this study,other studies have found education statistically significant in H.pylori seroprevalence [19,24,31].
As regards alcohol intake, our study showed no statistical significance in contrast to a study in Ethiopia [30] while in the Western World studies, alcohol intake was found protective [32] and especially so if taken in moderate amounts [33]. Alcohol is thought to eliminate H.pylori.
Thisstudy found no association between treatment of quality of drinking water and H. pyloriseropositivity in contrast to a study in Tanzania that found it an independent predictor of infectivity. The study in Tanzania found that participants that used untreated drinking water had 2.33 times the risk of getting H.pylori infection compared to those used treated water [18]. These differences would be due to differences in the geographical region and people's economic activity [34].
In this study seroprevalence in females was higher than in males but with no statistical significance.This trend of higher positivity in the female population was in agreement with a study in Mbarara Western Uganda [35] and in Kasese [17], but in contrast to ones in Cameroon [21] Canada [32] and Northern California [36]. However, a study in South Korea showed that being male was statistically associated with H. pylori positivity [31]. Females are reported to have a high tendency to clear the H. pyloridue to more frequent use of antibiotics than male [37]. Moreover the population of participants in Canada and Korea were different from those that participated in this study.
The seroprevalence of H.pylori infection in Eastern Uganda was high. Feeding on animal products was one of thepredisposing factors.
The Directorate of Graduate Studies, Research, and Innovations, Busitema University(DGSRI) funded data collection and manuscript writing but did not participate in conceptualisation, proposal writing and data analysis.
The authors extend their gratitude to the Department of Community and Public Health, Faculty of Health Sciences, Busitema University, Community Based Education and Research Services (COBERS) coordinator and Directorate of Graduate Studies, Research and Innovations, Busitema University, Kibuku district leadership, and respondents who participated on this study.
Citation: Rebecca Nekaka, Paul Oboth, Julius Nteziyaremye, Yahaya Gavamukulya, Lydia VN Ssenyonga, and Jacob Stanley Iramiot. Sero-Prevalence and Factors Associated with Helicobacter pylori Infection in a Rural Population in Eastern Uganda: A Community Cross-sectional Study. Prim Health Care, 2021, 11(4), 378
Received: 18-Mar-2021 Published: 30-Apr-2021, DOI: 10.35248/2167-1079.21.11.378
Copyright: © 2021 Nteziyaremye J, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.